The Vitamin Deficiency Affecting 40% of Seniors—And Why Your Doctor Might Miss It
Nearly one in five seniors experiences dangerously low vitamin D levels, yet most will never discover they have this deficiency. The reason is startling: current medical guidelines recommend against routine vitamin D testing for most adults, meaning this widespread problem often goes undiagnosed until serious complications develop.
More than 40% of American adults are vitamin D deficient, rising to 74% in older adults. Among frail hospitalized elderly patients, a staggering 87.4% show deficient levels.
The consequences extend far beyond bone health—affecting muscle strength, fall risk, immune function, cognitive performance, and cardiovascular health. This guide reveals why vitamin D deficiency remains so common in seniors, the subtle symptoms doctors attribute to “normal aging,” current testing controversies, and practical, evidence-based steps to address this silent crisis in 2025.
Why 3 Out of 4 Seniors Have Vitamin D Deficiency (And What You Can Do About It)
Your legs feel heavy when you climb stairs. You’re tired all the time. Your doctor says it’s just aging.
5 Symptoms Doctors Mistake for “Just Getting Older”
Check the symptoms you’re experiencing
Doctor Says:
“Normal Aging”
Could Actually Be:
“Vitamin D Deficiency”
Don’t assume it’s aging. These symptoms are often fixable with proper vitamin D levels.
If you checked 2+ boxes:
- Ask your doctor for a 25-hydroxyvitamin D test
- Mention your specific symptoms
- List your risk factors
But what if it’s not?
What if a simple vitamin deficiency is stealing your energy, weakening your muscles, and putting your bones at risk? And what if your doctor isn’t even testing for it?
Let’s talk about vitamin D deficiency in seniors. This isn’t some minor health issue. It’s affecting millions of older adults right now. And most don’t even know they have it.
The Numbers That Should Scare You (But Your Doctor Might Not Mention)
Here’s what the research shows. Over 40% of all adults are vitamin D deficient. That’s nearly half of everyone walking around.
But it gets worse for seniors.
Among older adults, 74% have inadequate vitamin D levels. Think about that. Three out of four seniors don’t have enough vitamin D in their bodies.
Globally, 59.7% of elderly people suffer from severe vitamin D deficiency. That’s not just low levels. That’s dangerously low.
And if you’re in a hospital or nursing home? About 87% of frail hospitalized elderly patients are deficient. Almost everyone.
The gender differences matter too. Elderly men show 44% rates of very severe deficiency compared to 26% in women.
Nearly 20% of seniors have dangerous vitamin D deficiency. Not just low. Dangerous.
Let’s break down what “deficiency” really means. Among middle-aged and older adults, 4.6% are severely deficient, 15.2% are moderately deficient, and 33.6% have insufficient levels. Add those up. That’s more than half of older people.
Geography plays a role too. In China, 70.3% of elderly people are deficient. In the US, it’s 17.4%. But even the lower US number means millions of seniors are affected.
Here’s the scary part. These aren’t just numbers on a lab report. Low vitamin D affects your bones, your muscles, your brain, and your immune system. It increases your risk of falls, fractures, infections, and even death.
Yet most doctors won’t test you for it.
Your Doctor Probably Won’t Test You. Here’s Why.
You might think with numbers this bad, doctors would test everyone. They don’t.
The Endocrine Society’s 2024 guidelines recommend against routine testing for healthy adults under 75. Read that again. They say don’t test.

The U.S. Preventive Services Task Force gives vitamin D screening an “I” statement. That means insufficient evidence. They’re not saying it’s bad to test. They’re saying they can’t prove it helps.
This creates a problem. You have symptoms. You might be deficient. But the guidelines say your doctor shouldn’t test you.
Why the change? Years ago, vitamin D testing was rare. Between 2005 and 2015 in the UK, vitamin D testing jumped from less than 1 test per 1,000 people to over 16 tests per 1,000 people.
In the US, Medicare reimbursement for vitamin D testing increased 80-fold from 2000 to 2010. That’s a lot of money. A lot of tests. And medical groups started asking: Does all this testing actually help people?
They decided it doesn’t. At least not for healthy people with no symptoms.
But here’s the catch. The guidelines focus on asymptomatic, healthy adults. That’s people with no symptoms and no risk factors. How many seniors does that really describe?
Most older adults have something going on. Medications. Chronic conditions. Mobility issues. The guidelines say these high-risk people might need testing. The USPSTF doesn’t recommend universal screening but acknowledges high-risk populations need evaluation.
The Symptoms Your Doctor Calls “Normal Aging”
Here’s what makes vitamin D deficiency so tricky. The symptoms are subtle and develop over years or even decades. They don’t hit you all at once. They creep up slowly.

You get tired. Your doctor says that’s normal for your age.
Your legs feel weak. That’s aging too, they say.
You’re more depressed. Well, getting older is hard, right?
Wrong. These could all be vitamin D deficiency. And they’re not normal. They’re fixable.
Let’s talk about what to watch for.
Your Muscles Feel Different
Muscle weakness shows up as heaviness in your legs, difficulty standing up from a chair, and trouble climbing stairs. You might notice you’re walking differently. Some people develop a waddling gait.

In severe cases, you get marked proximal muscle weakness. That means the muscles closest to your body—your thighs, your upper arms—stop working as well. You struggle with basic movements.
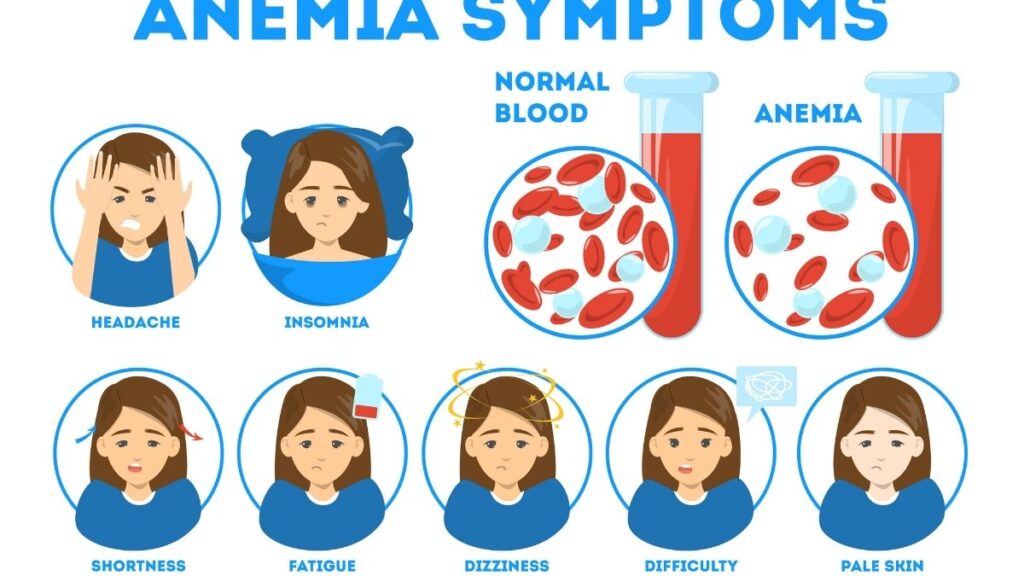
Your Mood Tanks
Mood changes including depression, fatigue, and cognitive decline are common. You feel down. Everything seems harder. You can’t think as clearly as you used to.
Vitamin D deficiency can cause delirium that looks like slowed thinking, confusion, and memory loss. Your family might think it’s Alzheimer’s disease. It might just be low vitamin D.
Everything Hurts
Bone pain, muscle pain, and increased fracture risk all connect to low vitamin D. Your bones ache. Your muscles hurt. You break bones more easily when you fall.

Severe aching in bones and muscles is a hallmark symptom. This isn’t just regular soreness. It’s deep, constant pain.
You Get Sick More Often
Frequent infections happen when vitamin D is low. You catch every cold. The flu hits you hard. Infections last longer.
You Fall More
Severe deficiency, with levels below 10 ng/mL, contributes to increased fall risk. Your balance gets worse. Your muscles don’t respond as quickly. You fall. And when you fall with weak bones, you break things.
Other Symptoms That Might Surprise You
Digestive issues and unexplained weight gain can also signal vitamin D problems.
Your risk for heart disease and high blood pressure goes up when vitamin D is low.
Here’s what you need to understand. These symptoms don’t happen overnight. They build slowly. You adjust to feeling worse. You think it’s just aging.
But it’s not. And you don’t have to live with it.
Why Seniors Get Hit the Hardest
Your body doesn’t make vitamin D as well as it used to. That’s not your fault. It’s biology.
As skin thins with age, vitamin D synthesis becomes much less efficient. The same amount of sunlight that worked when you were 30 doesn’t work at 70. Your skin can’t convert it as well.
You also have impaired intestinal absorption and impaired processing in your liver and kidneys. Even if you eat vitamin D or take supplements, your body struggles to use it properly.
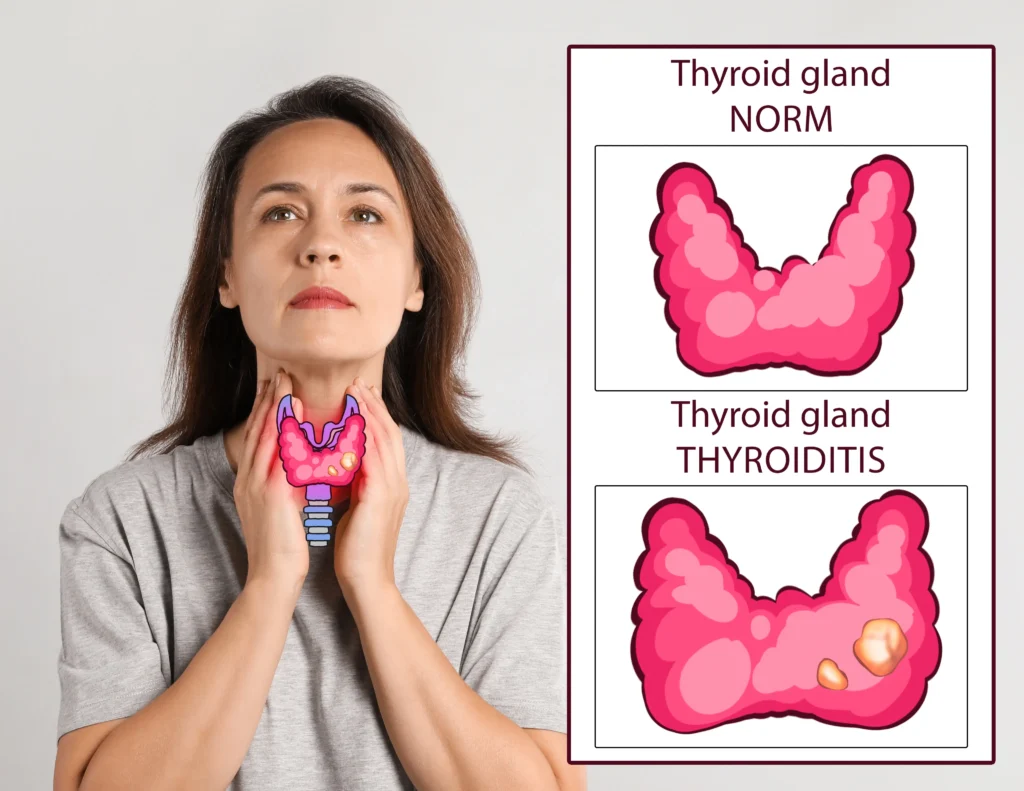
Your Stomach Acid Decreases
Up to 15% of seniors over 65 have hypochlorhydria, which means decreased gastric acid. You need stomach acid to absorb many nutrients, including vitamin D. Less acid means less absorption.

This happens with conditions like H. pylori infection, after some GI surgeries, and with certain digestive disorders. Drinking too much alcohol makes it worse.
You Stay Inside More
Mobility limitations keep seniors indoors. Maybe your knees hurt. Maybe you’re worried about falling. So you stay home. You don’t get sunlight. Your vitamin D levels drop.
Where You Live Matters
Northern latitudes have insufficient UV radiation during winter months. If you live in the northern US, Canada, or Europe, you can’t make vitamin D from sunlight for several months each year. The sun’s angle is wrong.
Your Body Shape Plays a Role
Research on body shape index shows an inverse relationship with vitamin D levels. How your body stores fat affects how much vitamin D you have available.
Medications Interfere
Many common medications affect vitamin D. We’ll cover this more in the next section. But if you take several medications—and most seniors do—your risk goes up.
Multiple Problems Stack Up
Think about it. Your skin works less well. Your gut absorbs less. Your kidneys process it less efficiently. You take medications that interfere. You stay inside more. You live in a place with less sun.

All these factors add up. That’s why seniors face such high deficiency rates. It’s not one thing. It’s everything happening at once.
The Medications Stealing Your Vitamin D (Check Your Medicine Cabinet)

Some of the medications you take every day might be draining your vitamin D. Your doctor might not have told you this.
Seizure Medications
Anticonvulsants like phenytoin, phenobarbital, primidone, and carbamazepine cause drug-induced osteomalacia. They interfere with how your body processes vitamin D. If you take these medications long-term, you’re at high risk.
Antibiotics and Other Common Drugs
Rifampin and some sleeping medications affect vitamin D metabolism. They change how your body breaks down and uses vitamin D.
Stomach Acid Reducers
You know those pills for heartburn and acid reflux? Calcium carbonate is poorly absorbed when you take PPIs or H2 blockers. These medications reduce your stomach acid. Remember how we said you need stomach acid to absorb nutrients? Less acid means less vitamin D absorption.
How Medications Interfere
Many drug-vitamin D interactions happen through interference with CYP3A4 activity. That’s an enzyme system in your liver. It helps process both medications and vitamin D. When medications take over that system, vitamin D processing suffers.
Steroids
Corticosteroids affect vitamin D metabolism. If you take prednisone or other steroids for conditions like arthritis, asthma, or autoimmune diseases, your vitamin D levels can drop.
The Statin Connection
Here’s something interesting. People taking statins who had muscle pain found that 92% got relief when their vitamin D deficiency was corrected. If you take cholesterol medications and have muscle pain, low vitamin D might be the cause.
Water Pills
Diuretics like furosemide show a complex relationship with vitamin D. They affect how your body handles calcium and vitamin D together.
What You Can Do
Don’t stop your medications. But talk to your doctor or pharmacist. Ask: “Do any of my medications affect vitamin D? Should I take extra vitamin D because of my medications?”
Many people need higher vitamin D doses when they take these drugs. But you need professional guidance to figure out the right amount.
When You Should Push for a Vitamin D Test
The guidelines say most people don’t need testing. But you’re not “most people” if you fit certain categories.

High-Risk Groups That Need Testing
Nursing home residents, older adults, women with osteoporosis, African American individuals, and Hispanic individuals should get screened.
Testing is also recommended for hospitalized patients, people with chronic kidney disease, chronic liver disease, and malabsorption syndromes.
Let’s be clear about what this means. If you:
- Live in a nursing home or assisted living
- Are over 65 (especially over 75)
- Have been diagnosed with osteoporosis
- Have darker skin (melanin reduces vitamin D production)
- Have kidney or liver disease
- Have Crohn’s disease, celiac disease, or had weight loss surgery
- Are in the hospital for any reason
You should ask for testing. The guidelines support it for you.
The Test You Need
The 25-hydroxyvitamin D test is the standard test. That’s what you ask for. Not “vitamin D.” Specifically “25-hydroxyvitamin D” or “25(OH)D.”
What the Numbers Mean
Levels below 20 ng/mL indicate deficiency. Levels between 20 and 30 ng/mL indicate insufficiency. Most experts now recommend getting your levels above 30 ng/mL. Optimal range is 30-50 ng/mL.
Here’s a sobering fact. Among people not taking vitamin D supplements, only 4.2% had desirable levels of 30 ng/mL or higher. Without supplements, almost nobody has good levels.
The Testing Problem
There’s no internationally recognized standard for vitamin D testing, and results vary by testing method. This is frustrating. But it doesn’t mean you shouldn’t test. It means you should use the same lab for follow-up tests to track your progress.
What’s More Important Than Testing
The most valuable screening tool is a thorough nutrition-focused history and physical exam. Tell your doctor about your diet. Your sun exposure. Your symptoms. Your medications. That information matters more than any guideline.
The Cost Issue
Insurance might not cover vitamin D testing for “routine screening.” But if you have risk factors or symptoms, coverage is more likely. You can also pay out of pocket. The test typically costs $40-$100 without insurance.
How to Ask Your Doctor
Don’t just say “Can I get a vitamin D test?” Say: “I have risk factors for vitamin D deficiency. I’m over 65, I take [list your medications], I stay inside most days, and I have symptoms like muscle weakness and fatigue. I’d like a 25-hydroxyvitamin D test.”
Be specific. Reference your risk factors. Most doctors will order the test when you explain why you need it.
The Foods That Actually Boost Vitamin D (Not Just Milk)

You can’t get all your vitamin D from food. But food helps. And some foods pack way more vitamin D than others.
The Fish That Win
Sockeye salmon has 570 IU per 3-ounce serving. Rainbow trout has 645 IU per 3 ounces.
Wild-caught salmon contains more vitamin D than farmed salmon. Baltic Sea salmon provides 556-924 IU per 3.5-ounce serving. That’s a big range, but even the low end is good.
Mackerel, sardines, and herring are also excellent choices. They’re often cheaper than salmon too.
The Surprising Powerhouse
One tablespoon of cod liver oil provides 227% of your daily vitamin D needs. That’s about 1,360 IU in just one tablespoon. Yes, it tastes bad. But it works.
Eggs and Meat
One large egg yolk contains 68 IU (1.7 mcg) of vitamin D. That’s not a lot, but eggs are easy to eat daily.
Beef liver has vitamin D too. Most people don’t eat it regularly, but if you do, it helps.
Fortified Foods Matter
Fortified foods provide most of the vitamin D in American diets. That means foods with vitamin D added to them.
One cup of fortified milk has 111-120 IU. Fortified orange juice has similar amounts. Some cereals are fortified with vitamin D.
Fortified cottage cheese also contains vitamin D. Check labels. “Fortified” means they added vitamins.
The Mushroom Trick
UV-treated mushrooms provide significant vitamin D. One cup can give you substantial amounts. Regular mushrooms have almost no vitamin D. But when mushrooms are exposed to UV light (some companies do this), they produce vitamin D. Look for labels that say “UV-treated” or “high in vitamin D.”
Building a Daily Food Plan
Let’s say you’re aiming for 800 IU per day from food. Here’s what that might look like:
- Breakfast: 2 eggs (136 IU) + 1 cup fortified milk (115 IU) = 251 IU
- Lunch: Tuna sandwich (154 IU for 3 oz tuna) + fortified yogurt (80 IU) = 234 IU
- Dinner: 3 oz salmon (570 IU) = 570 IU
Total: About 1,055 IU. You’d exceed your goal.
Or a budget-friendly version:
- Breakfast: Fortified cereal (80 IU) + fortified milk (115 IU) = 195 IU
- Lunch: Sardines on toast (200 IU for sardines) = 200 IU
- Dinner: Eggs and vegetables (136 IU for 2 eggs) = 136 IU
Total: 531 IU. Not bad, but you’d want to add a supplement.
The Reality Check
Most seniors struggle to get 800 IU from food alone. You’d need to eat fish multiple times per week. Not everyone likes fish. Not everyone can afford it. Not everyone can cook it regularly.
That’s okay. Get what you can from food. Then supplement the rest. The combination works best.
How Much Vitamin D You Actually Need (2025 Guidelines Made Clear)
Forget complicated advice. Here’s what the current guidelines say.
The Basic Recommendations
Adults under 70 need 600 IU daily. Adults 71 and older need 800 IU daily. Those are the Institute of Medicine (IOM) recommendations.
But there’s a catch. Adults 75 and older are now recommended to take vitamin D higher than the IOM daily allowance. Many experts say people over 75 should aim for 1,000-2,000 IU per day.
D3 vs. D2: Does It Matter?
Yes. Vitamin D3 is more effective than D2 for achieving optimal levels. When you buy supplements, look for “vitamin D3” or “cholecalciferol.” Avoid “vitamin D2” or “ergocalciferol.”
What Level to Aim For
Central European and Endocrine Society recommendations suggest targeting 30-50 ng/mL (75-125 nmol/L). That’s your goal range. Below 30 ng/mL, you’re not getting enough. Above 50 ng/mL, you don’t need more.
Is There Such a Thing as Too Much?
The maximum safe upper level is 4,000 IU daily for most adults. For obese adults, it’s 10,000 IU daily. You’d have to take a lot more than the recommended dose to reach toxic levels. But don’t go above 4,000 IU daily without medical supervision.
First-Line Treatment
Oral vitamin D3 and calcium together are the first-line therapy for deficiency. You need both. Vitamin D helps you absorb calcium. Calcium builds bones. They work together.
The Calcium Question
Take calcium carbonate with meals. If you’re on PPIs or acid reducers, take calcium citrate instead. Calcium citrate doesn’t need stomach acid to be absorbed.
How much calcium? Most experts recommend 1,000-1,200 mg per day for older adults. Split it into two doses. Your body absorbs it better that way.
Personalized Dosing Works Better
Treatment should be based on your actual 25(OH)D concentration, not blanket dosing. This means: get tested, see what your level is, then dose accordingly.
If your level is below 20 ng/mL, you might need 2,000-3,000 IU daily to get it up. If you’re at 25 ng/mL, maybe 1,000 IU daily is enough. Work with your doctor.
The Absorption Trick
Taking vitamin D with fat or fatty foods boosts absorption by 11-50%. Taking it with a large meal increases absorption by 50%.
Take your vitamin D with your fattiest meal. Eggs and bacon for breakfast? Perfect. Salmon for dinner? Great. Even just taking it with whole milk helps.
Don’t take it on an empty stomach. You’ll absorb much less.
Starting a Supplement
Buy vitamin D3. Start with 1,000-2,000 IU daily if you’re over 70. Take it with food that contains some fat. Take it at the same time every day so you remember.
Give it time. It takes 2-3 months to see changes in your blood levels. Don’t expect to feel different immediately.
Getting Vitamin D from Sunlight (Without Wrecking Your Skin)

Sunlight is the best natural source of vitamin D. Your skin makes it when UV rays hit your skin. But how do you balance vitamin D production with skin cancer risk?
How Much Sun You Need
For most people, 5-30 minutes of sunlight exposure twice weekly usually leads to adequate vitamin D production. That’s not much. Two or three times per week. Not even every day.
Half-body UV irradiation once weekly can increase vitamin D levels comparably to taking 800 IU daily. “Half-body” means exposing your arms and legs. You don’t need to sunbathe in a swimsuit.
The Aging Skin Problem
Skin synthesis becomes less efficient in older adults. You need more sun exposure than a 30-year-old to make the same amount of vitamin D. Your skin just doesn’t work as well.
Balancing Sun and Safety
You need to balance sun exposure benefits with skin cancer concerns. Here’s how to do it smart:
- Expose your arms and legs without sunscreen for 10-15 minutes
- Do this 2-3 times per week
- Choose times when the sun isn’t strongest (before 10 AM or after 4 PM)
- After your 10-15 minutes, apply sunscreen if you’re staying outside
- Don’t let your skin turn pink or burn
Geography and Seasons Matter
If you live in the northern US (above the latitude of Atlanta), you can’t make vitamin D from sunlight between November and February. The sun’s angle is too low. The UV rays don’t penetrate the atmosphere properly.
In those months, you need supplements. Sunlight won’t help.
For People Who Can’t Go Outside
For institutionalized elderly with mobility concerns, UV light therapy options exist. Some facilities use special UV lamps. They work like sunlight for vitamin D production. Ask if your care facility has this option.
The Bottom Line on Sun
A little sun helps. But don’t rely on it as your only source, especially if you’re over 70. Your skin doesn’t convert it well enough. Supplement too.
When Standard Treatment Doesn’t Work
Most people do fine with regular vitamin D supplements. But some people need different approaches.
Special Medical Conditions
People with liver failure, those on glucocorticoid treatment, and bariatric surgery patients need calcidiol. That’s a special form of vitamin D that bypasses some of the body’s conversion steps. Regular vitamin D won’t work well for them.
If you’ve had weight loss surgery, tell your doctor. You probably need higher doses or special forms of vitamin D.
Pernicious Anemia
If you have pernicious anemia, you need intrinsic factor support or B12 injections along with vitamin D treatment. These conditions often go together. Treating one without the other doesn’t work.
When Supplements Don’t Seem to Help
Here’s a frustrating reality. Even with supplementation, 44% of elderly patients remained deficient. Only 38% reached desirable levels.
Why? Sometimes you’re not taking enough. Sometimes you’re not absorbing it. Sometimes you have a medical condition interfering. Sometimes you need a different form of vitamin D.
If you’ve been taking supplements for 3-4 months and your levels haven’t improved, talk to your doctor. You might need:
- A higher dose
- A different form (prescription vitamin D)
- Testing for absorption problems
- Review of your medications
Depression and Vitamin D
Depression, measured by high GDS-15 scores, is associated with vitamin D deficiency. If you’re depressed, check your vitamin D. If your vitamin D is low, treating it might help your mood.
Muscle Weakness and Sarcopenia
Sarcopenia and muscle weakness require targeted vitamin D management. If muscle loss is your main problem, you might need higher doses of vitamin D combined with exercise and extra protein.
Don’t suffer in silence. If standard treatment isn’t working, there are other options.
What Vitamin D Deficiency Does Beyond Your Bones
Everyone knows vitamin D affects bones. But it does so much more.
Your Parathyroid Glands React
People over 75 often develop secondary hyperparathyroidism from vitamin D deficiency. Your parathyroid glands sense low calcium and vitamin D. They pump out extra parathyroid hormone. This pulls calcium from your bones to keep your blood calcium normal. Your blood tests look fine. But your bones are getting weaker.
Your Immune System Suffers
Vitamin D deficiency is linked to increased pneumonia mortality risk, with a hazard ratio of 3.82. That means people with low vitamin D are nearly four times more likely to die from pneumonia than people with normal levels.
You need vitamin D for your immune system to work properly. Low levels mean more infections, more severe infections, and longer recovery times.
Your Brain Is Affected
Low vitamin D links to increased Alzheimer’s disease and dementia risk. We don’t know if low vitamin D causes dementia or if dementia leads to behaviors that cause low vitamin D. But the connection is clear.
Your Heart Health
Cardiovascular problems and high blood pressure connect to low vitamin D. Your risk of heart disease, heart attacks, and strokes goes up when vitamin D is low.
Muscle Loss and Frailty
Sarcopenia, osteoporosis, and frailty syndrome all link to vitamin D deficiency. You lose muscle mass. Your bones weaken. You become frail. Falls happen more easily. Recovery takes longer.
This isn’t just about breaking a hip. It’s about your overall strength, independence, and quality of life.
The Whole-Body Picture
Think of vitamin D as a hormone, not just a vitamin. It affects almost every system in your body. When it’s low, everything suffers a little bit. When it’s optimal, everything works better.
Take Control of Your Vitamin D Status

Vitamin D deficiency affects 42% of all adults and 74% of older adults. Yet current guidelines discourage routine testing, creating a diagnostic gap.
Symptoms are subtle and often dismissed as normal aging. But they’re not normal. And you don’t have to accept them.
Multiple risk factors make seniors particularly vulnerable. Your skin. Your gut. Your medications. Where you live. How much you go outside. Everything adds up.
But solutions exist.
What You Can Do Starting Today
Talk to your doctor about vitamin D testing if you have risk factors. Be specific. Say: “I’m over 65. I have these symptoms. I take these medications. I want a 25-hydroxyvitamin D test.”
Start eating more vitamin D-rich foods. Add salmon to your weekly meals. Eat eggs for breakfast. Drink fortified milk. Every bit helps.
Consider a quality vitamin D3 supplement. Start with 1,000-2,000 IU daily. Take it with your fattiest meal. Discuss the exact dosage with your healthcare provider.
Spend 10-15 minutes outdoors daily when possible. Expose your arms and legs. Before 10 AM or after 4 PM is best. Then apply sunscreen if you’re staying out longer.
Review your medications with your pharmacist. Ask: “Do any of these affect vitamin D? Should I take extra vitamin D because of my medications?”
The Bottom Line
Don’t let vitamin D deficiency silently steal your health. You’ve spent your whole life taking care of your body. Don’t stop now.
Armed with this information, you can advocate for the testing and treatment you need. You can make dietary changes. You can supplement smart. You can get outside safely.
Your doctor might say you don’t need testing. But you know your body. You know your risk factors. Push back if you need to.
This isn’t about following guidelines. It’s about protecting your health, your strength, and your independence. That’s worth fighting for.