The Suffocating Truth: How Excess Weight Is Quietly Wrecking Your Lungs (And It’s Not Just COPD)
Taking a deep breath should be effortless, but for millions of people carrying excess weight, every inhale is a struggle against their own body. With 40% of American adults now obese, breathing difficulties have become an epidemic—yet most people don’t realize their weight is crushing their lung capacity.
Often misdiagnosed as asthma or dismissed as aging, these respiratory problems silently progress until permanent damage occurs. Understanding the connection between obesity and lung function is critical.
In this guide, you’ll discover exactly how excess weight damages your lungs, the specific warning signs you shouldn’t ignore, and proven weight loss strategies that can restore your breathing—including realistic timelines for when you’ll start feeling relief from weight-related breathing issues.
System Status
Summary placeholder.
DIAGNOSTIC DATA:
The Numbers That Should Scare You: What Obesity Does to Your Lungs

Your lungs are in trouble. And if you’re carrying extra weight, the damage might be worse than you think.
Right now, one billion people around the world are living with obesity. In the U.S., 40% of adults are obese. That’s not just a weight problem—it’s a breathing crisis.
Here’s what the research shows. If you’re obese, your chances of having breathing problems jump by 86.9%. That’s nearly double the risk. And if your weight sits mostly around your belly? Your risk shoots up by 84.2%.
Let’s talk about what this means for your lungs. In a study of middle-aged and older adults, 727 out of 5,631 people who were obese had a 12.3% lower chance of good lung function. That’s not a small difference. That’s the difference between walking up stairs without stopping and gasping for air halfway up.
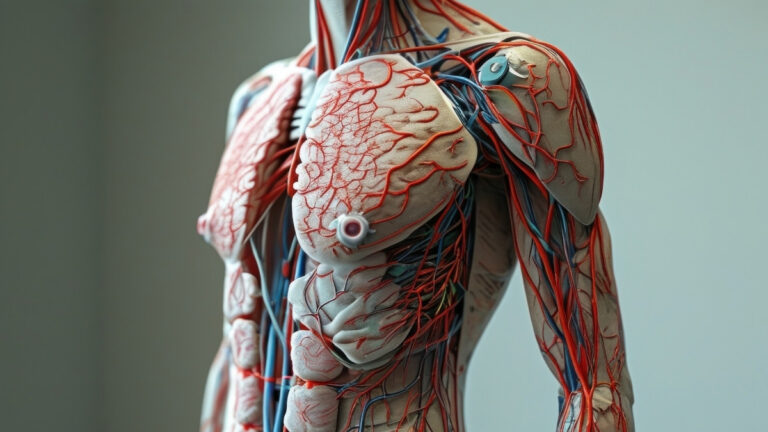
What 40 Pounds of Fat Does to Your Chest: The Physical Squeeze

Imagine someone sitting on your chest. All day. Every day. That’s basically what excess fat does to your lungs.
Here’s how it works. Fat doesn’t just sit on your body looking bad. It pushes and squeezes. When fat builds up on your chest wall, it presses down on your rib cage. Can’t expand properly? Can’t breathe properly.
The fat in your belly does something even worse. It pushes your diaphragm up. Your diaphragm is the main muscle that helps you breathe. When fat shoves it upward, it can’t move like it should. You end up working harder for every breath.
Let’s look at the actual numbers. Your lungs have different volumes—think of them like the capacity of a water tank. When you gain weight, here’s what happens:
Expiratory Reserve Volume (ERV) drops first. This is the extra air you can push out after a normal breath. It falls exponentially as your BMI goes up. In fact, once you hit a BMI of just 25—that’s barely into the “overweight” category—your ERV already falls below normal.
Functional Residual Capacity (FRC) can drop by 30-40% if you’re severely obese. This is how much air stays in your lungs between breaths. Less air means less oxygen reserve.
Total Lung Capacity (TLC) shrinks by up to 20% when your BMI hits 40 or higher. That’s one-fifth of your breathing capacity, gone.
For every 10-point increase in BMI, men lose 1.4% of their lung capacity. Women lose 0.9%. That might sound small, but add it up over 20 or 30 BMI points. You’re talking about serious loss.
One study showed something amazing. Women who lost just 7.5 pounds from their chest wall saw their lung volumes improve. Just 7.5 pounds.
Where you carry the weight matters too. Belly fat (doctors call it android obesity) crushes your lungs the worst. Fat on your hips and thighs? Not as bad for breathing, though it’s still not great for you.
The Silent Attack: How Fat Cells Release Chemicals That Choke Your Airways

Fat doesn’t just squeeze your lungs from the outside. It attacks them from the inside too.
Here’s what most people don’t know. Your fat tissue isn’t just storage. It’s an organ. An active one. And it’s pumping out chemicals that hurt your lungs every single day.
Fat cells release inflammatory molecules. Think of inflammation like a small fire burning inside you all the time. This fire reaches your airways and makes them angry and reactive.
The main players? Leptin goes up. This hormone messes with your lung’s defenses. Adiponectin goes down. This one actually protects your lungs, so losing it is bad news. TNF-alpha and IL-6 both increase. These drive inflammation throughout your body, including your airways.
Your airways become hyperresponsive. That means they overreact to everything. Dust, cold air, exercise—things that shouldn’t bother you suddenly trigger breathing problems. It’s similar to asthma but not exactly the same.
Actually, obesity creates two different types of asthma. If you had asthma as a kid (the allergic type), obesity makes it worse. But obesity can also cause brand-new asthma in adults—a different kind that’s driven by weight and inflammation, not allergies.
There’s something called metabolic syndrome. It’s a cluster of problems: high blood sugar, high blood pressure, bad cholesterol. Guess what? Your belly fat drives this syndrome. And this syndrome hurts your lungs even more. It’s a compound effect—one problem making another problem worse.
Your immune system takes a hit too. High leptin levels weaken your lung’s ability to fight infections. You get sick more often. You stay sick longer. You end up in the hospital more.
Obese patients show increased markers of inflammation in their lung fluid. Their airways are under constant attack, even when they feel fine.
This isn’t visible damage. You can’t see it on a regular X-ray. But it’s happening. Your fat is waging a chemical war on your ability to breathe.
Why You Can’t Catch Your Breath: The Low Lung Volume Trap

Ever feel like you’re suffocating even though you’re breathing? There’s a reason for that.
Your lungs normally rest at a comfortable volume between breaths. This is called your Functional Residual Capacity. It’s your breathing baseline. Your safety cushion.
Obesity steals this cushion.
When your FRC drops, you’re forced to breathe near the bottom of your lung range. You’re operating at the absolute minimum. There’s no room for error. No reserve for when you need it.
Here’s where it gets worse. Small airways in your lungs start to collapse. These are tiny tubes deep in your lungs. When you’re breathing at such low volumes, they close up during normal breathing.
This creates a mismatch—blood flows to areas that aren’t getting air. Your oxygen levels drop even though you’re breathing.
The numbers tell the story. Obese women use 27 mL more oxygen just to breathe during exercise compared to lean women. That’s oxygen that should go to your muscles. Instead, it’s being wasted on the act of breathing itself.
Think about it like this. You’re trying to run a race, but 16-27% of your energy goes to just breathing. Not running. Not moving. Just breathing. No wonder you’re tired.
And it creates a terrible cycle. Exercise is hard → You need more oxygen → Your breathing muscles steal that oxygen → You have less for your muscles → Exercise feels even harder → You stop exercising → You gain more weight.
Position matters too. Lying down makes everything worse. Gravity pulls your belly contents up against your diaphragm. Your maximum breathing strength drops significantly. This is why sleep problems are so common with obesity.
One study showed something hopeful, though. After just 8% weight loss, the oxygen cost of breathing dropped by 16%. Your body became 16% more efficient at the basic act of breathing. That’s the difference between struggling and managing.
How Your Weight Is Suffocating You at Night

You know that feeling of gasping awake in the middle of the night? That’s your body screaming for oxygen.
70% of people with sleep apnea are obese. If your BMI is over 30, your risk of sleep apnea is four times higher than someone at a healthy weight.
Here’s what happens. Fat deposits build up around your upper airway—your throat, tongue, and soft tissues. When you lie down and relax during sleep, these tissues collapse. They block your airway.
You stop breathing. Your brain panics and wakes you up just enough to gasp for air. Then you fall back asleep and it happens again. And again. And again. Sometimes hundreds of times per night.
Some people develop something even worse called Obesity Hypoventilation Syndrome. This affects 10-20% of severely obese people. Your body stops getting rid of carbon dioxide properly, even during the day.
One patient lost 50 pounds and went from using a CPAP machine every night to not needing it at all. The breathing pauses stopped. The gasping stopped. The exhaustion stopped.
Your weight is literally suffocating you while you sleep. But you can fix it.
The Best News You’ll Read Today: How Losing Weight Fixes Your Lungs

Here’s something amazing. Your lungs can heal. Studies from 2020 to 2025 show the same thing over and over. When you lose weight, your lungs get better. It doesn’t matter if you lose it through diet, exercise, or surgery. It works.
And you don’t need to lose massive amounts of weight to see changes.
Lose 5-8% of your body weight (that’s 10-16 pounds if you weigh 200). Your Expiratory Reserve Volume jumps up by 18-25%. Your breathing mechanics during exercise improve. The oxygen cost of breathing drops by 16%. You feel the difference within weeks.
Lose 10-13% (20-26 pounds at 200). Your lung capacity improves by 92 mL for every 10% you lose. Your breathing tests show real, measurable improvements. Your total lung capacity increases by 3-5%.
Lose more than 13% and the improvements become dramatic. People who lose significant weight see their lung function approach normal levels. Tests that were failing start passing.
The timeline matters. In the first four weeks, you’ll notice you’re not as breathless. Sleep gets better. Within 6-12 weeks, actual lung volume measurements improve. By six months, you’ve got substantial restoration of function.
Your 8-Week Plan to Breathe Easier
Your 8-Week Plan to Breathe Easier!
Week 1: Assess Where You Are
- Calculate your BMI using any free online calculator.
- Measure your waist at your belly button.
- Write down every time you get breathless (climbing stairs, tying shoes, etc.).
- Buy a peak flow meter ($15-30) and track your breathing every morning.
Weeks 2-3: Fix Your Food
- Cut 500-750 calories per day (e.g., one less soda, smaller portions).
- Eat 25-30 grams of fiber daily (berries, veggies, beans).
- Add anti-inflammatory foods (leafy greens, nuts, fatty fish).
- Get enough protein to protect muscle (0.8g per kg of body weight).
- Cut way back on processed foods.
Weeks 4-6: Start Moving
- Start with 5-10 minutes of walking every day. Build slowly.
- Add 2-3 minutes each week. Aim for 20-25 minutes by week 8.
- Avoid high-traffic areas (pollution) when exercising. Find a park.
- Add resistance training twice a week (bodyweight squats, push-ups, lunges).
Weeks 7-8: Level Up
- Increase walking to 25-30 minutes daily. Add a second walk if you can.
- Track your progress: weigh yourself weekly, use your peak flow meter.
- Notice when stairs get easier!
- Consider inspiratory muscle training (devices that strengthen breathing muscles).
Breathing Exercises (Start Today!)
Pursed-Lip Breathing
- Breathe in through your nose (2 counts).
- Purse lips (like blowing a candle).
- Breathe out slowly (4 counts).
- Do 5-10 minutes daily.
Diaphragmatic Breathing
- Lie on your back, hand on belly.
- Breathe in so your belly rises (not your chest).
- Do 10 breaths, three times per day.
- Strengthens your main breathing muscle.
Goals & Daily Checklist
Daily Checklist
- Track meals & stay in calorie target.
- Walk your daily minutes.
- Do one breathing exercise session.
- Get 7-9 hours of sleep.
- Avoid smoking & vaping.
Realistic Goals
- Aim for 5-10% body weight loss over 6 months.
- Weigh yourself once a week (same day, same time).
- Measure breathing monthly (stairs climbed, distance walked).
Get Medical Help If…
- You are snoring loudly or gasping for air at night (get a sleep study).
- Your BMI is over 35 and you have breathing symptoms.
- Your asthma is getting worse as you gain weight.
- You’re trying everything and still struggling (ask about medications or surgery).
Stop reading and start doing. Here’s exactly what to do.
Week 1: Assess Where You Are
Calculate your BMI today. Use any free online calculator. Measure your waist at your belly button. Write down every time you get breathless this week—climbing stairs, walking to your car, tying your shoes. Notice the patterns.
If you can, buy a peak flow meter. They cost $15-30 at any pharmacy. Test your breathing every morning. Track the numbers.
Weeks 2-3: Fix Your Food
Cut 500-750 calories per day. Not a crazy diet. Just less. One less soda. Smaller portions. Skip the late-night snack.
Eat 25-30 grams of fiber daily. Fiber helps lung function. Berries, vegetables, whole grains, beans. Get creative.
Add anti-inflammatory foods. Berries. Leafy greens. Nuts. Fatty fish. These help calm down the inflammation in your airways.
Get enough protein—0.8 to 1 gram per kilogram of body weight. This protects your muscles while you lose fat.
Cut way back on processed foods. They drive inflammation. Your lungs hate them.
Weeks 4-6: Start Moving
Start with 5-10 minutes of walking. Every day. Too easy? Good. Build slowly.
Add 2-3 minutes each week. No rush. By week 8, you should hit 20-25 minutes.
Avoid high-traffic areas when exercising. Pollution makes breathing problems worse. Find a park. Walk in your neighborhood during off-peak hours.
Add resistance training twice a week. Bodyweight exercises work fine. Push-ups, squats, lunges. Keep it simple.
Start These Breathing Exercises Today
Pursed-lip breathing (do this right now):
- Breathe in through your nose for 2 counts
- Purse your lips like you’re blowing out a candle
- Breathe out slowly through pursed lips for 4 counts
- Do this for 5-10 minutes daily
- Use it when you’re breathless
Diaphragmatic breathing (before bed):
- Lie on your back
- Put one hand on your belly
- Breathe so your belly rises, not your chest
- 10 breaths, three times per day
- Strengthens your main breathing muscle
Weeks 7-8: Level Up
Increase walking to 25-30 minutes daily. Add a second daily walk if possible. Morning and evening works great.
Track your progress. Weigh yourself weekly. Test your breathing with the peak flow meter. Notice when stairs get easier.
Consider inspiratory muscle training. Special devices exist that make your breathing muscles stronger. 15-30 minutes, 3-5 times per week. The research shows they help.
Get Medical Help If:
You’re snoring loudly or gasping at night → Get a sleep study Your BMI is over 35 with any breathing symptoms → See a doctor Your asthma is getting worse as you gain weight → Talk to your doctor You’re trying everything and still struggling → Ask about weight loss medications or surgery
The Daily Checklist
- Track your meals and stay in your calorie target
- Walk your daily minutes
- Do one breathing exercise session
- Drink enough water
- Get 7-9 hours of sleep
- Avoid smoking and vaping (they make everything worse)
Set Realistic Goals
Aim for 5-10% body weight loss over 6 months. If you weigh 200 pounds, that’s 10-20 pounds. Totally doable.
Weigh yourself once a week. Same day, same time, same scale.
Measure your breathing monthly. Count how many stairs you can climb without stopping. Time how far you can walk without getting breathless.
Celebrate every 5 pounds lost. Celebrate every breathing improvement. You earned it.
This isn’t a temporary diet. This is how you live now. Your lungs are depending on you.
Red Flags That Mean Call Your Doctor Now

Some symptoms need immediate attention. Don’t ignore these.
Early Warning Signs (see your doctor this week):
- You’re breathless climbing just one flight of stairs
- You can’t talk while walking at a normal pace
- You wake up gasping for air
- You get morning headaches regularly
- You’re sleepy all day despite getting enough time in bed
Progressive Problems (see your doctor today):
- You need to sleep propped up on multiple pillows to breathe
- Your ankles are swelling (sign your heart is struggling)
- Your lips or fingernails look bluish
- You’re confused or having memory problems
- You have chest pain or pressure
Emergency Symptoms (call 911):
- Severe shortness of breath while resting
- Rapid breathing that you can’t slow down
- Your lips are turning blue
- You’re confused or can’t think clearly
- Chest pain plus breathing difficulty
Don’t Wait If:
- Your breathing problems are new or getting worse
- You suspect you have sleep apnea
- Your BMI is over 35 and you have any respiratory symptoms
- You have asthma that’s getting worse as you gain weight
Tests Your Doctor Might Run:
Spirometry measures your lung volumes. You blow into a machine and it tells you how well your lungs work.
Pulse oximetry clips to your finger and measures oxygen in your blood.
Arterial blood gas checks your CO₂ levels with a blood draw.
Sleep study monitors you overnight to catch breathing pauses.
Chest X-ray or CT scan looks at your lung structure.
Echocardiogram uses ultrasound to check how your heart is handling the strain.
None of these tests hurt. All of them give valuable information about what’s happening in your lungs.
The key point: breathing problems with obesity are serious. They’re not just part of being overweight. They’re warning signs your body needs help.
Don’t tough it out. Don’t wait until it’s an emergency. Your lungs are too important.
Here’s What You Need to Remember
Your weight is crushing your lungs. Literally pressing down on them. Making them smaller. Making every breath harder.
But it’s not just physical pressure. Your fat tissue is releasing inflammatory chemicals that attack your airways from the inside. Creating a constant state of irritation and hyperreactivity.
The good news? Everything I just described is reversible. Lose just 5-10% of your body weight and you’ll see measurable improvements. Your lung volumes increase. Your breathing gets easier. The inflammation calms down.
The changes start within weeks. Not months. Weeks.
The combination of smart eating, regular movement, and breathing exercises works better than any one approach alone. You need all three.
Don’t wait for a medical emergency to take action. Your lungs are calling for help right now.
Start with one thing. One walk today. One breathing exercise session. Swap one processed meal for whole foods. Track your BMI. Note one breathing difficulty you’re experiencing.
Every small step moves you toward easier breathing and better health.
Thanks for reading! I hope this was helpful. See you next time. Bye-bye!