Joint Lubrication: Eat Your Way Out of Arthritis – The Anti-Inflammatory Fats That “Oil” Your Knees
Imagine reducing your arthritis pain by nearly 30% without a single pill, just by changing the oils in your kitchen. Nearly 60 million American adults live with arthritis, with 24.3% experiencing daily pain that disrupts their lives.
Many depend on NSAIDs for relief, but these medications carry long-term risks, including gastrointestinal damage and cardiovascular concerns. The solution may be simpler than you think. Specific anti-inflammatory fats for arthritis can act like natural joint lubricants, reducing inflammation from within.
This guide reveals which omega-3 fatty acids support joint health, practical ways to incorporate these healing foods daily, and which fats you must avoid because they worsen inflammation.
The Science of Inflammation and Joint Pain
Food Pharmacy
Salmon & Sardines
Pack the most EPA/DHA. Aim for 2-3 servings/week. One 3oz salmon fillet has 1,500mg (more than daily need).
Your joints are sending you a message. That morning stiffness, the ache when you climb stairs, the swelling that won't quit—it's all connected to one thing: inflammation.
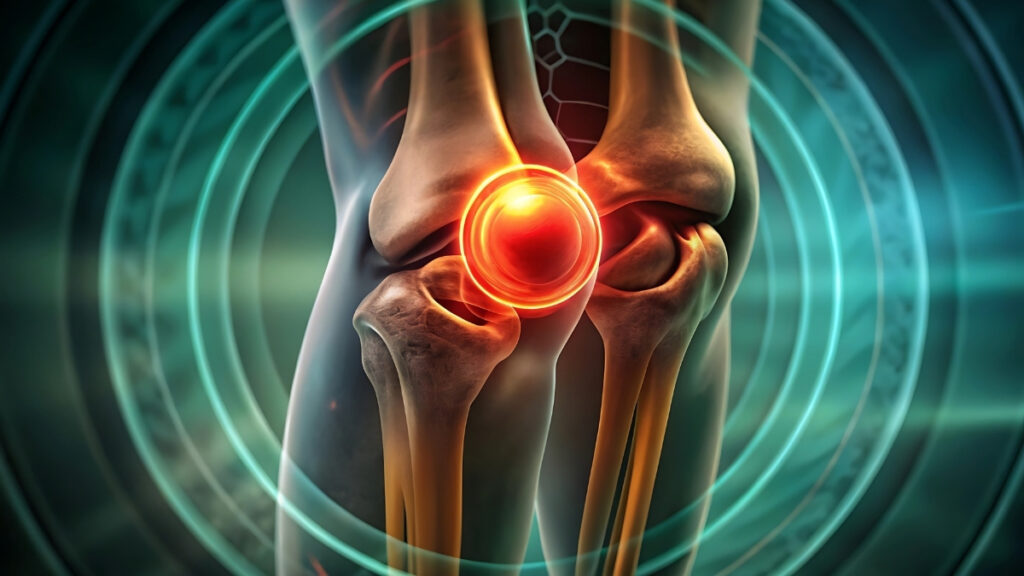
How Inflammation Attacks Your Joints

Think of inflammation like a fire inside your joints. When this fire burns too long, it destroys the cushioning between your bones. Your body releases proteins called cytokines—specifically IL-1β, TNF-α, and IL-6. These aren't just medical terms. They're the chemicals that eat away at your cartilage, piece by piece.
Here's what makes it worse: chronic inflammation doesn't just damage tissue. It makes your nerves more sensitive to pain. That's why joints that used to feel fine now hurt constantly. The inflammation turns up your pain volume.
And if you're carrying extra weight, there's more bad news. Fat tissue isn't just sitting there. It actively creates inflammatory chemicals called adipokines. These spread through your bloodstream and attack joints all over your body—even joints that don't bear weight, like your hands.
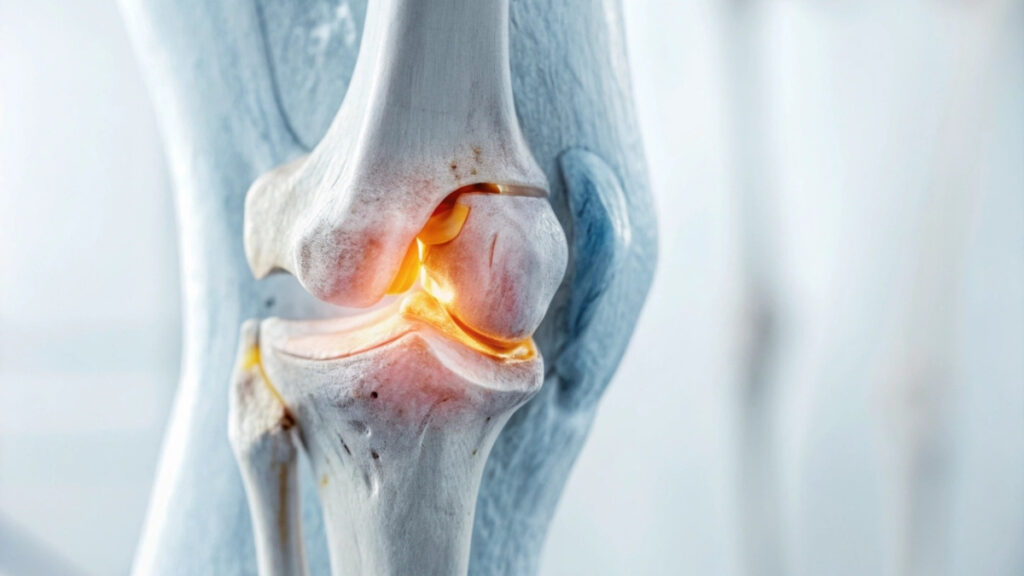
The Oil Change Your Body Needs

Your joints need healthy fats the same way your car needs clean oil. When you eat the right fats, they work like anti-inflammatory medicine in your body.
Studies show that healthy fats reduce inflammatory markers in your blood—things like CRP and interleukin-6. These are the same markers doctors test to measure inflammation. After one month of eating healthy fats, inflammation drops noticeably. By six months, the improvement is significant.
How does this work? Healthy fats block the same inflammatory pathways that ibuprofen blocks—COX-1 and COX-2 enzymes. But unlike pills, these fats come from food. No prescriptions needed.
The Weight Connection You Need to Know

Here's a fact that sounds made up but isn't: losing just one pound removes four pounds of pressure from your knees. That's because of how joints work when you move. Every step multiplies the force on your knees.
But weight affects more than just pressure. Remember those adipokines we mentioned? The more fat tissue you have, the more inflammatory chemicals your body makes. This is why people with arthritis in their knees often have pain in their hands too. The inflammation spreads.
Research proves this connection matters. If you reduce your BMI by more than 13% over five years, you have a 74% chance of slowing down joint damage in your knees. That's not a small improvement. That's life-changing.
Breaking the Inflammation Cycle

The cytokine cascade sounds complicated, but it's simple. One inflammatory protein triggers another, which triggers another. It's like dominoes falling. Healthy fats stop the cascade by blocking key enzymes early in the chain.
This is similar to how ibuprofen works, but natural. COX enzymes create prostaglandins—the chemicals that cause pain and swelling. When you eat anti-inflammatory fats regularly, they reduce COX activity. Less COX means fewer prostaglandins. Fewer prostaglandins means less pain.
The best part? You'll notice the difference. Not overnight, but within weeks. Your joints will feel less stiff. Movement becomes easier. The constant ache starts to fade.
Your body is designed to heal itself. Sometimes it just needs the right fuel to do the job.
Omega-3 Fatty Acids: Your Joints' Best Friend
If you could take one supplement that actually works for joint pain, omega-3s would be it. Not because of marketing hype. Because of what the research shows.
The Evidence That Proves It Works

Another review focused specifically on osteoarthritis patients—2,070 people across nine studies. Omega-3s significantly reduced pain and improved how well joints worked. People could move better. They hurt less.
Here's the surprising part: lower doses worked better than higher doses. Studies found that 1.35 grams per day or less was more effective than taking more. Your body can only use so much at once.
The benefits show up most strongly for rheumatoid arthritis and mixed chronic pain. For osteoarthritis alone, some studies show benefits while others don't. But when you combine all the evidence, omega-3s help more people than they don't.
Which Type of Omega-3 Matters Most
Not all omega-3s are equal. EPA (eicosapentaenoic acid) shows the strongest anti-inflammatory effects for joints. DHA helps too, but EPA is the star player.
You need 600 to 1,000 milligrams daily. You can get this from food or supplements. Food is better because you get other nutrients too, but supplements work if you don't eat fish.
Plant sources give you ALA (alpha-linolenic acid). Your body converts some of this to EPA, but not much. You'd need to eat a lot of flaxseeds to match the EPA in one serving of salmon.
The Best Food Sources

Fatty fish tops the list. Salmon, mackerel, sardines, herring, and anchovies pack the most omega-3s. Aim for two to three servings each week.
One 3-ounce serving of salmon gives you about 1,500 milligrams of EPA and DHA combined. That's more than your daily target in one meal. Sardines are even better gram for gram, plus they're cheap and loaded with calcium.
Plant sources matter too. Ground flaxseeds, chia seeds, walnuts, and hemp seeds all provide omega-3s. Sprinkle ground flaxseed on oatmeal. Toss walnuts in salads. Blend chia seeds into smoothies.
But here's what most people miss: the ratio between omega-6 and omega-3 fats matters as much as the total amount. Americans eat way too many omega-6s (from vegetable oils and processed foods) and not enough omega-3s. Aim for a ratio of 3:1 or lower.
Simple Ways to Get More Omega-3s

Start your day with oatmeal topped with ground flaxseed and walnuts. That's omega-3s right there, plus fiber to keep you full.
For lunch, make a salad with canned salmon or sardines. Mix in olive oil and lemon juice. Add vegetables. You just hit your omega-3 target and got anti-inflammatory polyphenols from the olive oil.
Dinner could be grilled mackerel with roasted vegetables. Or baked salmon with quinoa and steamed broccoli. Simple meals that taste good and reduce inflammation.
Keep walnuts in your desk or car. A small handful (about an ounce) gives you 2.5 grams of ALA. That's a solid snack that fights joint pain while you work.
Olive Oil's Secret Weapon: Oleocanthal
You probably have a bottle of olive oil in your kitchen right now. What you might not know is that it contains a natural painkiller called oleocanthal. And it works.
The Ibuprofen Hiding in Your Pantry

Oleocanthal blocks the same enzymes that ibuprofen blocks—COX-1 and COX-2. These enzymes create inflammation and pain. When you stop them, you reduce both.
Here's the dose comparison: about four tablespoons of quality olive oil gives you oleocanthal equal to 10% of an adult ibuprofen dose. That might not sound like much, but you're eating this daily, not just when pain strikes.
Good olive oil has a peppery bite that stings your throat slightly. That's the oleocanthal. If your olive oil tastes bland and smooth, it doesn't have much oleocanthal. The sting tells you it's working.
How to Choose the Right Olive Oil

Not all olive oil is created equal. You need extra virgin olive oil—EVOO for short. This is the first pressing of the olives, with no heat or chemicals used. It keeps all the beneficial compounds intact.
Tuscan varieties and early harvest oils contain the most oleocanthal. Look for harvest dates on the bottle. The fresher, the better. Olive oil loses its polyphenols over time.
Cold-pressed and unrefined matter too. Heat and processing destroy the delicate compounds that fight inflammation. Quality EVOO might cost more, but you're buying medicine, not just cooking oil.
About 30 different polyphenols exist in olive oil. They all work together to reduce inflammation and protect your cells from damage. Oleocanthal is the star, but the supporting cast helps too.
Monounsaturated Fats: The Joint Protectors
The Joint Mechanic
Rusty Joints?
Inflammation acts like rust. Cytokines (proteins) eat away cartilage cushioning. Without healthy fats, joints grind painfully.
Monounsaturated fats fly under the radar compared to omega-3s. But they deserve your attention. These fats protect your joints in ways that even omega-3s can't match.
Avocado and Avocado Oil Benefits
:max_bytes(150000):strip_icc()/Health-GettyImages-974251806-bee639463a554149a83565ac50221759.jpg)
Avocados are packed with oleic acid—the same type of fat that makes olive oil healthy. Oleic acid reduces inflammation markers throughout your body.
But avocados offer something unique: ASU, or avocado/soybean unsaponifiables. Don't let the name scare you. ASU reduces osteoarthritis pain and stiffness. It works by protecting cartilage and slowing down the breakdown process.
ASU has three properties that help joints: it protects existing cartilage (chondroprotective), it helps build new cartilage (anabolic), and it prevents cartilage destruction (anticatabolic). That's a triple threat against arthritis.
Avocados also contain vitamin E and beta-sitosterol. Vitamin E is an antioxidant that protects cells. Beta-sitosterol is a plant compound that fights inflammation. You get all of this in one food.
Avocado Oil for Cooking

Avocado oil has a high smoke point—around 520°F. This means you can use it for stir-frying, sautéing, and even roasting without breaking down the beneficial fats.
The flavor is mild. It won't overpower your food like some oils do. You can use it anywhere you'd use vegetable oil, but you'll get anti-inflammatory benefits instead.
Cold-pressed avocado oil retains more nutrients than refined versions. Look for "cold-pressed" or "expeller-pressed" on the label. Avoid "pure" avocado oil—it's often mixed with cheaper oils.
Other Beneficial Oils
Walnut oil deserves special mention. It contains 10 times more omega-3s than olive oil. Use it in salad dressings or drizzle it over finished dishes. Don't cook with it—the omega-3s break down with heat.
The flavor is nutty and slightly bitter. A little goes a long way. Mix it half and half with olive oil if the taste is too strong.
Other good options include macadamia nut oil and hazelnut oil. Both provide monounsaturated fats and unique flavors. They're pricier, but you don't need much.
Practical Ways to Use Monounsaturated Fats

Start with breakfast. Add half an avocado to your eggs or oatmeal. Weird? Maybe. Effective? Definitely. Use avocado oil for your lunch stir-fry. Toss vegetables in the hot pan. The oil won't smoke or turn bitter. Your joints get protection while you get a tasty meal.
Make a simple guacamole: mashed avocado, lime juice, salt, and diced tomatoes. Eat it with veggie sticks or whole grain chips. You just ate joint medicine that tastes like a snack.
For dinner, drizzle walnut oil over roasted Brussels sprouts or steamed green beans. The nutty flavor complements vegetables perfectly.
Turmeric and Curcumin: The Golden Anti-Inflammatory
Walk into any health food store and you'll see turmeric everywhere. The hype is justified. This golden spice actually works for joint pain, and the research proves it.
The Clinical Evidence Is Strong

A 2023 analysis looked at 23 studies with 2,175 patients. Curcumin (the active compound in turmeric) significantly reduced pain. It also improved WOMAC scores—a standard test that measures pain, stiffness, and function in people with arthritis.
Another review in 2025 examined all types of turmeric preparations. Every single one reduced pain significantly. The effects ranged from moderate to large, depending on the preparation and dose.
Fifty studies conducted between 2004 and 2024 confirmed curcumin's anti-inflammatory effects. It also protects cells from damage and prevents cell death. That matters because dead cartilage cells can't repair themselves.
How Curcumin Fights Joint Pain
Curcumin blocks the same inflammatory proteins that destroy your joints—cytokines like IL-1β, TNF-α, and IL-6. It also inhibits COX-2 enzymes, just like ibuprofen does.
But curcumin does something NSAIDs can't: it reduces joint swelling by stopping prostaglandin production at multiple points in the inflammatory pathway. It's like cutting off a fire's oxygen supply at several locations instead of just one.
Studies comparing curcumin to NSAIDs found something interesting. Curcumin causes fewer side effects. NSAIDs can damage your stomach and kidneys with long-term use. Curcumin doesn't.
The Absorption Problem and How to Fix It
Here's the catch: your body absorbs curcumin poorly. Eat a spoonful of turmeric powder, and most of it passes through undigested.
Black pepper solves this problem. Specifically, a compound in black pepper called piperine increases curcumin absorption by 2,000%. That's not a typo. Twenty times better absorption.
Add a pinch of black pepper to any dish with turmeric. Problem solved. This is why Indian cuisine traditionally combines turmeric and black pepper in curries.
Fat helps too. Curcumin dissolves in fat, not water. Take your curcumin supplement with a meal that contains fat. Or mix turmeric powder into full-fat coconut milk for golden milk.
Effective Doses and Timeline

Studies showing benefits used 500 to 1,500 milligrams of curcumin daily. Most turmeric supplements list the curcumin content on the label. Regular turmeric powder is only about 3% curcumin by weight.
Treatment periods of four to six months show the best results. Don't expect overnight miracles. Curcumin needs time to reduce inflammation and protect cartilage.
Take it consistently. Missing days reduces effectiveness. Think of it as medication, not an occasional supplement.
Simple Ways to Use Turmeric Daily
Add a teaspoon of turmeric powder to scrambled eggs. The color is bright, but the flavor is mild. Sprinkle in some black pepper and you're done.
Make golden milk before bed: heat one cup of milk (dairy or plant-based), stir in half a teaspoon of turmeric powder, a pinch of black pepper, a tiny bit of ginger, and honey to taste. This is an ancient remedy that modern science validates.
Toss turmeric into soups and stews. It adds color and anti-inflammatory power without changing the taste much. Start with a quarter teaspoon and increase gradually.
Blend turmeric into smoothies. Half a teaspoon won't affect the flavor if you're using fruits and greens. Add a pinch of black pepper and some nut butter for fat.
Supplements vs. Food

Supplements give you higher, more consistent doses. Look for products that include piperine or "bioperine" (a patented form of piperine extract). Check the curcumin content—you want at least 500 milligrams per capsule.
Some supplements use liposomal curcumin or curcumin bound to phospholipids. These absorb better without needing black pepper. They cost more but work well.
Fresh turmeric root works too. It looks like small ginger roots with bright orange flesh. Grate it into dishes or juice it. Wear gloves—it stains everything.
What to Expect
After four weeks of consistent use, you might notice slightly less pain. By eight weeks, the improvement becomes clearer. Stiffness decreases. Movement feels easier.
Maximum benefits appear around three to six months. That's when cartilage protection really kicks in and inflammation drops significantly.
If you stop taking curcumin, benefits fade within weeks. This isn't a cure. It's management. But it's effective management with minimal side effects.
Turmeric earned its place in traditional medicine over thousands of years. Now modern research explains why it works. Give it time and pair it with black pepper. Your joints will respond.
Other Anti-Inflammatory Superfoods for Joints
You don't need exotic supplements to fight joint pain. Regular foods from the grocery store pack serious anti-inflammatory power. Add these to your weekly rotation.
Colorful Berries and Fruits

Blueberries, cherries, and strawberries contain anthocyanins—pigments that give berries their deep colors. These compounds fight inflammation through antioxidant action.
Cherries deserve special attention. Studies show tart cherry juice reduces arthritis pain and stiffness. The effect comes from both anti-inflammatory compounds and natural melatonin that improves sleep.
Citrus fruits—oranges, grapefruits, lemons—provide vitamin C. Your body needs vitamin C to make collagen, a key component of cartilage and connective tissue. One orange gives you 100% of your daily vitamin C needs.
Eat berries fresh, frozen, or dried. Frozen berries are picked at peak ripeness and frozen immediately, so they're just as nutritious as fresh. Toss them into oatmeal, yogurt, or smoothies.
Cruciferous Vegetables Fight Inflammation Hard

Broccoli, kale, Brussels sprouts, and cauliflower contain sulforaphane—a compound that dramatically reduces inflammatory markers in your blood.
These vegetables are also packed with vitamin K. Studies link vitamin K intake to lower arthritis rates and better bone health. One cup of cooked kale gives you 10 times your daily vitamin K requirement.
The catch? You need to eat them regularly. Occasional broccoli won't do much. But half a cup daily makes a measurable difference.
Roast cruciferous vegetables with olive oil and garlic. The heat brings out the sweetness you don't get from steaming. Or sauté them quickly in avocado oil to preserve the sulforaphane.
Leafy Greens: Simple but Powerful
Spinach, Swiss chard, collard greens, and arugula offer anti-inflammatory benefits without the strong taste of cruciferous vegetables.
Raw spinach in salads works. But cooking it concentrates nutrients. You can eat way more cooked spinach than raw because it wilts down to nothing. One cup of raw spinach becomes about a quarter cup cooked.
Mix different greens for variety. Arugula has a peppery bite. Chard is mild. Collard greens taste heartier. Rotate them so you don't get bored.
Add greens to everything: scrambled eggs, soups, pasta, smoothies, stir-fries. They're hard to overcook and easy to hide if you don't love the taste.
Ginger Root Works Like Medicine

Ginger has anti-inflammatory properties similar to ibuprofen. It reduces joint pain and swelling through multiple mechanisms—blocking inflammatory enzymes, reducing oxidative stress, and interfering with pain signals.
Fresh ginger is stronger than dried. Peel it, grate it, and add it to stir-fries, soups, or tea. One-inch piece of fresh ginger equals about one teaspoon grated.
Ginger tea is simple: slice fresh ginger, steep in hot water for 5 to 10 minutes, add honey and lemon. Drink this daily for consistent anti-inflammatory effects.
Ginger supplements work too. Studies use 250 to 500 milligrams daily. Take them with food to avoid stomach upset.
Garlic and Onions Protect Cartilage

Allium vegetables—garlic, onions, leeks, shallots—contain organosulfur compounds that reduce inflammation and limit cartilage-damaging enzymes.
Studies show people who eat more alliums have lower arthritis rates. The effect isn't huge, but every bit helps when you're fighting joint pain.
Raw garlic is most potent. Crush it and let it sit for 10 minutes before cooking—this activates the beneficial compounds. Then cook it gently. High heat destroys some benefits.
Don't like raw garlic? Roast whole bulbs until soft and sweet. Squeeze the cloves onto bread or mix them into mashed potatoes. You get a milder flavor but still get anti-inflammatory benefits.
Building These Into Your Week
- Monday: Berry smoothie with spinach and flaxseed for breakfast
- Tuesday: Roasted broccoli and cauliflower with olive oil for dinner
- Wednesday: Ginger tea in the afternoon, garlic-heavy stir-fry at night
- Thursday: Kale salad with citrus dressing and cherry tomatoes
- Friday: Brussels sprouts with onions, tart cherry juice before bed
You don't need all of these every day. But aim for berries or citrus daily, cruciferous vegetables three to four times weekly, and ginger or garlic most days.
These foods work together. The anti-inflammatory effects add up. Your joints feel the difference when you eat this way consistently for weeks and months.
Nobody expects you to love every food on this list. Pick three you can tolerate and eat those regularly. That's better than forcing yourself to eat foods you hate. Consistency beats perfection.
Foods to Avoid: The Inflammation Triggers
Fighting inflammation isn't just about adding good foods. You also need to reduce foods that trigger inflammation. Here's what hurts your joints.
Added Sugars and Refined Carbohydrates

Sugar triggers the release of inflammatory messengers called cytokines. The same proteins that destroy cartilage. Every time you eat sugar, you're feeding inflammation.
White bread, pasta, cookies, cakes, and sugary drinks all spike your blood sugar quickly. This spike triggers an inflammatory response. Do this repeatedly and inflammation becomes chronic.
Health experts recommend keeping added sugars below 10% of your daily calories. For a 2,000-calorie diet, that's 50 grams max—about the amount in one 16-ounce soda.
Check labels. Sugar hides under dozens of names: high fructose corn syrup, cane juice, dextrose, maltose, and more. If it ends in "-ose," it's sugar.
Saturated and Trans Fats Fuel Inflammation

Red meat, full-fat dairy, butter, and cheese contain saturated fats. These trigger adipose tissue (fat cells) to release inflammatory chemicals.
Trans fats are worse. They're found in partially hydrogenated oils used in many processed foods. Trans fats strongly promote inflammation and have no safe level of consumption.
This doesn't mean eliminating all animal fats. It means choosing carefully. Grass-fed beef has a better fat profile than grain-fed. Wild salmon beats farmed. Small changes matter.
Replace saturated fats with healthy fats, not with more carbs. Swap butter for olive oil. Choose avocado instead of cheese. Grill fish instead of steak.
Highly Processed Foods Pack Multiple Triggers

Processed foods contain multiple inflammation triggers in one package: added sugars, refined oils, trans fats, and artificial additives.
They're also loaded with omega-6 fatty acids without balancing omega-3s. The ratio matters. Too much omega-6 relative to omega-3 promotes inflammation.
Hidden sugars in processed foods add up fast. "Healthy" granola bars often contain more sugar than cookies. Read labels. If sugar is in the first three ingredients, skip it.
Frozen dinners, packaged snacks, fast food, and processed meats (hot dogs, deli meat, bacon) all drive inflammation. Save these for occasional treats, not daily staples.
The Omega-6 Problem
Omega-6 fatty acids aren't inherently bad. Your body needs some. But Americans eat way too much—mostly from corn oil, soybean oil, and processed foods made with these oils.
The ideal ratio of omega-6 to omega-3 is around 3:1. Most Americans eat a ratio of 15:1 or higher. This imbalance promotes inflammation.
Avoid cooking oils high in omega-6: corn oil, soybean oil, cottonseed oil, and generic "vegetable oil." Use olive oil, avocado oil, or coconut oil instead.
Restaurant food and packaged foods almost always use cheap omega-6 oils. Cook at home when possible. You control what oils you use.
Simple Food Swaps That Work
- Instead of white bread: Eat whole-grain bread with seeds
- Instead of ice cream: Try Greek yogurt with fresh berries
- Instead of fried chicken: Bake or grill fish
- Instead of cookies: Snack on a handful of walnuts
- Instead of soda: Drink water with lemon or unsweetened tea
- Instead of chips: Munch on carrot sticks with hummus
These swaps reduce inflammation triggers while adding anti-inflammatory nutrients. You're not just removing bad foods—you're replacing them with good ones.
What About Treats?
Nobody eats perfectly. That's fine. The goal is making better choices most of the time.
The 80/20 rule works: eat anti-inflammatory foods 80% of the time. The other 20%? Live your life. One cookie won't destroy your joints. But a cookie every day for months will.
Special occasions deserve special food. Birthday cake at parties? Go for it. But don't buy a cake every week and call it a special occasion.
Seeing Results
When you cut inflammatory foods, you might notice improvements within two weeks. Less morning stiffness. Slightly better mobility. Less swelling.
By four to six weeks, the changes become obvious. Pain decreases. Energy improves. You realize how much those foods were affecting you.
If you eat inflammatory foods again, symptoms return. This isn't psychological. It's how inflammation works. Bad foods trigger it. Good foods reduce it.
You can't out-supplement a bad diet. All the fish oil in the world won't overcome daily soda and donuts. Fix your diet first. Supplements second.
Your joints are waiting for you to stop hurting them. Every meal is a choice. Choose foods that fight inflammation instead of causing it.
Your Journey Starts Now
Reducing joint pain through anti-inflammatory fats for arthritis starts with your next meal. Not next week. Not after you finish the junk food in your pantry. Now.
Go to your kitchen. Find your olive oil. If it's cheap and tasteless, order better stuff tonight. If you don't have walnuts, add them to your shopping list.
Small actions compound. Every meal that reduces inflammation is a meal that helps your joints heal. Every day you choose anti-inflammatory fats is a day you're fighting back against arthritis.
Your joints are waiting. They're ready to feel better. Give them the fats they need, and they'll respond. Start today.