It’s Not Just Sugar: The Seemingly Innocent Vegetable Worsening Your Inflammation (And What to Eat Instead)
You replaced processed foods with vegetables, started eating ‘clean,’ and somehow still wake up with joint pain, bloating, or brain fog. What’s going on? Not all vegetables are created equal for everyone.
While nightshade vegetables and certain other Rupa Health produce don’t cause inflammation in most people, they may worsen existing inflammatory conditions in sensitive individuals. In this guide, you’ll discover the four main categories of vegetables that worsen inflammation, backed by 2024-2025 research.
You’ll learn how to identify your personal triggers through food sensitivities testing, understand your body’s inflammatory response, and find powerful anti-inflammatory vegetable alternatives that actually support your health goals.
The Inflammation Veggie Guide!
Green Zone
Eat Freely!Yellow Zone
Moderate PortionsRed Zone
Consider CautionNot All “Healthy” Vegetables Are Anti-Inflammatory for Everyone

Most people can eat any vegetable without problems. But if you have arthritis, psoriasis, IBS, or other inflammatory conditions, some vegetables might make your symptoms worse.
Here’s what scientists have found:
Certain vegetables contain compounds called glycoalkaloids. These can irritate your gut lining and trigger immune responses in sensitive people. Think of it like how some people can pet cats without sneezing, while others start sniffling immediately. Same cat, different reaction.
The Arthritis Foundation says there’s no proof that nightshade vegetables cause arthritis in everyone. But individual responses vary wildly.
Dr. Childers’ research showed something interesting. Between 74% and 90% of people with chronic pain might be sensitive to nightshades. That’s not everyone. But it’s not rare either.
A 2024 study is testing this for the first time in a proper clinical trial. Researchers are looking at whether eliminating certain vegetables reduces inflammation markers in people with rheumatoid arthritis.
Food sensitivities aren’t the same as allergies. You won’t break out in hives or stop breathing. Instead, you might feel tired, achy, or bloated for hours or days after eating.
The tricky part? Your body’s response is personal. What bothers your friend might be fine for you.
4 Types of Vegetables That May Worsen Your Inflammation
Nightshades: The Most Controversial Inflammation Trigger

Nightshade vegetables belong to the Solanaceae family. They contain compounds called alkaloids, mainly solanine and capsaicin.
Common nightshades include:
- Tomatoes
- White potatoes
- Eggplant
- Bell peppers (all colors)
- Hot peppers
- Cayenne, paprika, and chili powder
In high amounts, these compounds can mess with your gut lining. They may increase intestinal permeability, which means stuff that should stay in your digestive tract can leak into your bloodstream.
For some people with IBS or inflammatory bowel disease, nightshades make symptoms worse.
But here’s where it gets confusing. A 2024 study on rats found mixed results. One part suggested solanine might actually protect joints and lower inflammation in osteoarthritis. Another part found increased inflammation markers.
Why the contradiction? Because biology is messy. What happens in a lab doesn’t always match what happens in your body. And what happens in rat bodies doesn’t always match human bodies.
Green or sprouting potatoes have the highest solanine content. If your potatoes look green, toss them. Cooked tomatoes in pasta sauce are still nightshades. The cooking doesn’t remove the alkaloids.
Some people cut out nightshades for six weeks and feel amazing. Others notice zero difference. The only way to know is to test it yourself.
The Hidden Sodium Problem in Canned Vegetables
Canned vegetables contain six to eight times more sodium than fresh or frozen ones.

A single serving of canned black beans has 459mg of sodium. That’s 20% of your daily limit. Fresh vegetables? Usually under 50mg per serving.
High sodium doesn’t just raise blood pressure. It can make inflammation worse.
Your kidneys work hard to balance sodium levels. When you eat too much salt, your body holds onto water to dilute it. This puts stress on your cardiovascular system and can trigger inflammatory responses.
Good news: You can fix this easily.
Draining canned vegetables cuts sodium by 36%. Rinsing them reduces it by 41%. Even better, look for cans marked “low sodium” or “no added salt” with 200mg or less per serving.
In 2025, most brands offer low-sodium versions. They taste nearly identical to the regular ones once you season them yourself.
If you’re dealing with inflammation, fresh or frozen vegetables are your best bet. But if you use canned, rinse them first.
FODMAP Vegetables That Trigger Gut Inflammation
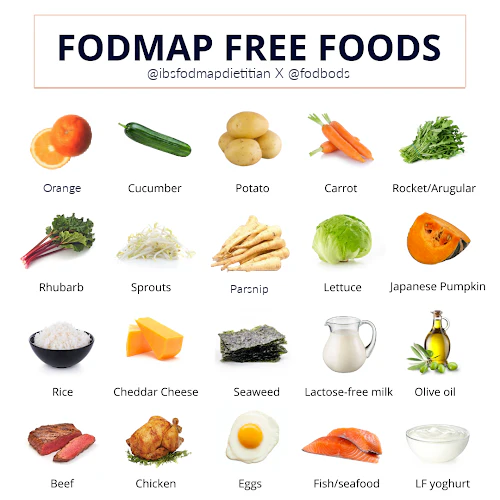
FODMAP stands for fermentable oligosaccharides, disaccharides, monosaccharides, and polyols. That’s a mouthful. Here’s what it means:
These are types of carbohydrates found in certain vegetables. Your small intestine struggles to absorb them. When they reach your large intestine, bacteria feast on them and produce gas.
For people with IBS, this causes bloating, cramping, and other digestive issues. A National Institutes of Health study found that 86% of IBS patients got substantially better following a low-FODMAP diet.
High-FODMAP vegetables include:
- Onions
- Garlic
- Cauliflower
- Mushrooms
- Asparagus
- Brussels sprouts
- Cabbage
Onion and garlic are the worst offenders. Even “healthy” vegetables like broccoli and asparagus can trigger symptoms.
For people with inflammatory bowel disease like Crohn’s, nightshades and high-FODMAP vegetables can cause abdominal pain. That’s why elimination diets for Crohn’s often remove both.
Here’s the weird part: Portion size matters. You might handle a few pieces of asparagus fine but feel terrible after eating a full plate. Your tolerance can change based on stress, sleep, and what else you ate that day.
How Cooking Method Turns Healthy Vegetables Inflammatory
This one surprises people. The vegetable isn’t the problem. It’s how you cook it.

Vegetables fried in omega-6 rich oils become pro-inflammatory. These oils include canola, corn, soybean, and sunflower oil.
Our ancestors ate omega-6 and omega-3 fats in roughly equal amounts. Today, the ratio is 10:1 or even 25:1 in favor of omega-6.
When you heat oils high in linoleic acid (an omega-6 fat), it oxidizes. This creates compounds called OXLAMs – oxidized linoleic acid metabolites. Scientists have linked OXLAMs to fibromyalgia, fatty liver disease, and atherosclerosis.
Think about:
- French fries
- Tempura vegetables
- Fried zucchini
- Vegetable chips (most are fried)
- Restaurant vegetables (usually cooked in cheap oils)
The vegetables themselves are fine. Potatoes, zucchini, and peppers aren’t inherently inflammatory. But fry them in the wrong oil, and you’ve created something your body struggles with.
The fix is simple. Use extra virgin olive oil, avocado oil, or coconut oil instead. These oils handle heat better and don’t create the same inflammatory compounds.
3-Step Process to Discover Which Vegetables Trigger YOUR Inflammation
Your 21-Day Inflammation Detective Guide!
Become your own health detective! Follow this weekly guide to uncover food sensitivities and calm inflammation. Let’s solve the case!
What to Eliminate
Symptoms to Track Daily
How to Reintroduce Foods
Success Markers Checklist
- Followed elimination phase strictly.
- Kept a detailed symptom journal.
- Identified specific trigger foods (if any).
- Experienced reduced inflammation symptoms.
- Established a sustainable, anti-inflammatory eating pattern.
Step 1: Elimination Phase (2-6 Weeks)
Remove all suspected vegetables for at least two weeks. Six weeks is better if you can manage it.
Keep a food and symptom diary. Write down:
- What you eat
- How you feel (energy, digestion, pain, mood)
- Sleep quality
- Skin condition
Be specific. "Felt bad" doesn't help. "Sharp pain in left knee at 3pm" does.
Look for patterns. Do you wake up feeling less puffy? Does your brain fog clear? Can you move more easily?
Step 2: Reintroduction Phase (6-8 Weeks)
Now add back one food at a time. Eat a small portion and wait three days before trying the next one.
Why three days? Because some reactions show up immediately. Others take 48 hours or more.
Start with the vegetables you miss most. If you love tomatoes, test those first. If you can't tolerate them, at least you know.
Document everything. Did you feel fine? Great. Did you feel worse? That's valuable information too.
Step 3: Personalization Phase (Ongoing)
Create your own list of what works and what doesn't. This becomes your personal eating guide.
You might find you can handle cooked tomatoes but not raw ones. Or that you tolerate small amounts of garlic powder but not fresh garlic. Or that bell peppers are fine but jalapeños aren't.
Food sensitivities can change over time. Your gut health improves. Stress decreases. What bothered you last year might be fine now. Check in with yourself every few months.
15 Powerhouse Anti-Inflammatory Vegetables to Eat Instead

While you're figuring out your triggers, load up on vegetables that fight inflammation.
Leafy Greens
Spinach and kale pack natural antioxidants and polyphenols. These compounds protect your cells from damage and reduce inflammation.
Cruciferous Vegetables
A 2024 study found that people who ate more cruciferous vegetables had 12% to 24% lower levels of inflammatory markers in their blood.
Good options:
- Broccoli (in moderation if you're FODMAP-sensitive)
- Bok choy
- Arugula
- Radishes
Colorful Vegetables
Red, purple, and dark blue vegetables contain anthocyanins. These pigments fight inflammation by neutralizing free radicals and reducing oxidative stress.
Try:
- Beets
- Red cabbage (if you tolerate FODMAP vegetables)
- Purple carrots
Root Vegetables
Sweet potatoes, carrots, and turnips are nutrient-dense and generally well-tolerated. Skip white potatoes if you're testing nightshade sensitivity.
Low-FODMAP Champions
If you have IBS, stick with:
- Bell peppers (yes, these are nightshades, but they're low-FODMAP)
- Bok choy
- Carrots
- Cucumber
- Kale
- Lettuce
- Spinach
- Zucchini
- Green beans
- Swiss chard
- Celery
- Pumpkin
- Winter squash
Most of these vegetables are safe to eat daily unless you have a specific sensitivity to them.
How to Reduce Inflammation from Vegetables: 7 Actionable Strategies

1. Choose Fresh Over Canned
Or rinse canned vegetables for 30 seconds under cold water. This simple step cuts sodium by 41%.
2. Use Anti-Inflammatory Cooking Oils
Switch to extra virgin olive oil for most cooking. Use avocado oil for high-heat cooking. Try coconut oil for roasting.
3. Try Different Preparation Methods
Peeling tomatoes and potatoes may reduce alkaloid content. Some people tolerate these vegetables better without the skin.
4. Watch Portion Sizes
Even vegetables you tolerate can cause problems in large amounts. Start with smaller servings and see how you feel.
5. Pair Strategically
Eat vegetables with omega-3 rich foods like salmon, walnuts, or flaxseeds. This helps balance your omega-6 to omega-3 ratio.
6. Consider Cooking Methods
Cooked vegetables are often easier to digest than raw ones. Cooking also makes some nutrients more bioavailable, meaning your body can use them better.
Steaming, roasting, and sautéing are gentler than frying.

7. Work with a Professional
A registered dietitian can guide you through an elimination diet properly. They'll make sure you're still getting all the nutrients you need while testing foods.
This matters because cutting out entire food groups without guidance can lead to deficiencies.
The Great Veggie Swap!
Your Next Steps
Most vegetables are healthy. But nightshades, high-FODMAP vegetables, high-sodium canned options, and those fried in inflammatory oils may worsen symptoms in sensitive people.
The key word is "may." Not "will."
Your body is unique. Your inflammatory response is unique. An anti-inflammatory diet loaded with fruits, vegetables, whole grains, nuts, and healthy fats works for most people. But you need to find your personal version of it.
Start with a three-week elimination of suspected trigger vegetables. Track your symptoms in a journal. Notice improvements in energy, digestion, or pain levels.
Your body will tell you what it needs. You just have to listen.
Understanding which vegetables worsen inflammation for your unique body lets you create a truly anti-inflammatory diet that supports your health goals. It's not about eating perfectly. It's about eating what makes you feel good.