I Ignored the Symptoms of Chronic Sleep Deprivation for 5 Years: The Metabolic and Cardiovascular Debt I Paid
Lucas lived under the illusion of high productivity, believing he could outmaneuver biology by consistently sacrificing rest. This choice, clinically known as chronic sleep deprivation, became a mounting debt, described by experts as a “high-interest loan with steep payments”.
The constant exhaustion, coupled with dangerously slowed reaction times and severe trouble focusing, was not a minor inconvenience but a systemic threat. Like millions of other adults, Lucas failed to meet the required seven to nine hours of restorative sleep.
A near-miss accident while driving served as the crisis point, forcing him to recognize his lack of rest was actively destroying his body. This article outlines Lucas’s descent and the actionable, clinical roadmap he followed to recover his health and cognitive vitality.
The Debt Crisis: Systemic Damage from Chronic Sleep Loss
The High-Interest Loan of Sleep Deprivation
Chronic sleep loss is not just being tired; it’s a systemic biological threat. Experts call it a “high-interest loan with steep payments,” where sacrificed rest actively triggers a state of physiological warfare.
- The Lie: That you can outsmart biology through sheer willpower.
- The Cost: Systemic destruction impacting heart, brain, and metabolism.
Pillar 1: Cardiovascular Collapse ❤️
Chronic sleep debt causes constant stress (cortisol), leading to elevated blood pressure and arterial stiffness.
- Risk Stat: Sleep deprivation is linked to a **48% increased risk of developing heart disease.
- Quality Matters: Fragmented sleep (insomnia) is associated with a **13% to 22% higher risk of cardiovascular disease.
Pillar 2: Metabolic Chaos & Diabetes Risk 🍎
Poor sleep rewires your hunger hormones, increasing Ghrelin (hunger) and lowering Leptin (satiety).
- Obesity Risk: Less than 5 hours of sleep nightly leads to a 50% higher risk for obesity.
- Diabetes Risk: Chronic insufficient sleep nearly triples the risk for developing Type 2 Diabetes.
Pillar 3: Cognitive Breakdown 🧠
Chronic sleep loss is a measurable contributor to neuro-degenerative risk, leading to structural brain changes.
- Brain Aging: Chronic sleep deprivation can age the brain by an estimated 3 to 5 years.
- Dementia Risk: Dementia risk increases by 33% due to chronic sleep debt and lack of deep (SWS/REM) sleep.
The Recovery Roadmap: CBT-I Pillars 🛠️
The gold standard for recovery is Cognitive Behavioral Therapy for Insomnia (CBT-I), which addresses underlying behavior, not just symptoms. It relies on four pillars:
- **Pillar 1 (SET): Focus on Quality over quantity of time in bed.
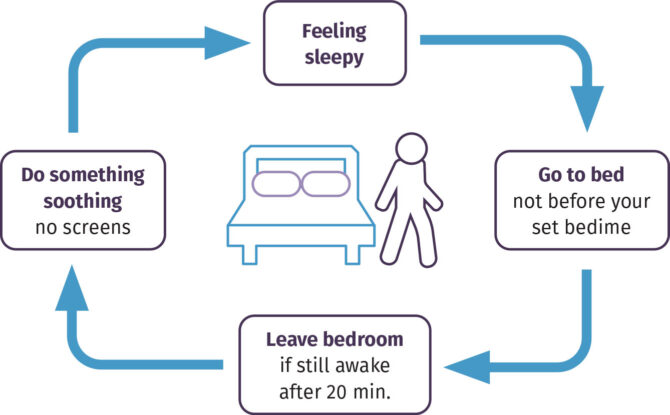
- **Pillar 2 (SCT): Break the association between bed and wakefulness (The 20-Minute Rule).
- **Pillar 3 (CT): Manage the “racing mind”** and reframing negative thoughts.
- **Pillar 4 (SH): Maintain a consistent wake-up time** every day.
The Ultimate Reward: Longevity and Clarity ⏳
The damage is largely reversible with consistent, high-quality sleep. Consistent, optimal sleep directly translates to years of extended life.
- **Longevity Gain (Men): Optimal sleep adds an average of +4.7 years to life expectancy.
- Longevity Gain (Women): Optimal sleep adds an average of +2.4 years to life expectancy.
The Crisis Point: When the High-Interest Loan Came Due

The story of chronic sleep loss often begins not with a dramatic collapse, but with a simple, insidious belief: that one can outsmart biology through sheer willpower.
Many individuals, driven by ambitious careers or overwhelming personal responsibilities, operate under the fallacy of productivity, equating less time sleeping with more time achieving.
This choice, however, is not a lifestyle hack; it is clinically described as chronic sleep deprivation, or insufficient sleep repeatedly over time, which experts liken to taking a "high-interest loan with steep payments".
For many years, the daily toll of this debt seemed minor, manifesting only as daytime tiredness, slower reaction times, and general trouble focusing.
The severity of this issue becomes tragically clear when one realizes the immediate impact on critical, high-stakes decision-making.
Researchers studying cognitive impairment have confirmed that blunted reactions to feedback while sleep-deprived can underlie critical failures, especially in dynamic environments requiring rapid adaptation to uncertainty.
For instance, investigations into major public safety disasters, including the 1979 nuclear accident at Three Mile Island, the 1986 Chernobyl nuclear meltdown, and even the explosion of the space shuttle Challenger, have concluded that sleep deprivation among key decision-makers played a significant, critical role.
When personal fatigue culminates in a near-miss—such as falling asleep briefly while driving or making a catastrophic, costly error at work—it represents the moment the high-interest loan of sleep debt comes due, threatening not just the individual's life but the stability of their professional and family world.
The Debt Statement: Systemic Destruction and Clinical Proof

The damage caused by ignoring the fundamental need for rest is systemic, triggering physiological changes that mimic chronic disease. When the body is repeatedly deprived of sleep, it activates a state of physiological warfare.
The systemic response involves the body interpreting sleep loss as constant stress, leading to the hyperactivation of the central stress response systems—specifically the Sympathetic Nervous System (SNS) and the Hypothalamic-Pituitary-Adrenal (HPA) axis.
This constant state of alert, mediated by stress hormones like cortisol, drives systemic inflammation, which is the root cause of the body's breakdown across multiple organ systems.
Cardiovascular Collapse: The Heart Under Siege

The constant elevation of stress hormones due to chronic sleep debt directly contributes to cardiovascular disease. The physiological mechanisms observed include the hyperactivation of the HPA axis, which leads to the elevation of basal blood pressure and contributes significantly to arterial stiffness.
Over time, this chronic hypertension dramatically increases the risk of serious cardiovascular events, including stroke and death.
Clinical research reinforces the extreme danger of sustained sleep loss. Chronic sleep deprivation is robustly linked to a 48% increased risk of developing heart disease.
Furthermore, the danger extends beyond just the quantity of sleep; the quality is an equally important, non-negotiable factor in determining cardiovascular outcomes.
Studies have shown that difficulty initiating sleep, difficulty maintaining sleep, or having consistently nonrestful sleep (common symptoms of insomnia) are associated with a significantly higher risk of cardiovascular disease, ranging from a 13% to 22% increased risk depending on the specific insomnia complaint.
This heightened risk means that even individuals who technically spend eight hours in bed but whose sleep is fragmented or nonrestorative are still putting their heart health at serious risk.
Metabolic Chaos: Rewiring Hunger and Diabetes Risk
Sleep deprivation profoundly disrupts metabolic health, primarily by interfering with the delicate balance of appetite-regulating hormones.
Poor sleep patterns cause an endocrine shift that increases levels of Ghrelin, often called the hunger hormone, while simultaneously lowering levels of Leptin, the hormone responsible for signaling satiety or appetite control.
This imbalance directly leads to increased cravings for sweet, salty, and savory foods and promotes overeating and subsequent weight gain.
The consequences of this metabolic chaos are severe. Individuals who consistently get less than five hours of sleep nightly face a 50% higher risk for obesity. The link to diabetes is even more pronounced, with chronic insufficient sleep nearly tripling the risk for developing Type 2 Diabetes (T2DM).
Compounding this, studies indicate a U-shaped relationship between sleep duration and T2DM risk, meaning that both abbreviated (too little) and extended (too much) sleep are linked to a higher probability of developing the condition.
Defining metabolic terms like insulin resistance and Type 2 diabetes clearly is essential for the reader, ensuring that the connection between sleep and these life-altering conditions is understood as a direct, physiological threat.
Cognitive Breakdown: Aging the Brain 3-5 Years
The brain is highly vulnerable to sleep loss, with immediate consequences including depression, anxiety, irritability, fuzzy thinking, and increased forgetfulness.
While these are recognized short-term effects, the long-term structural changes are even more alarming. Research shows that chronic sleep deprivation can age the brain by an estimated three to five years.
Current studies have established that suboptimal sleep duration is significantly correlated with indicators of poor brain health. These indicators include silent brain injuries, such as white matter hyperintensities, which clinicians recognize as forewarning stroke and dementia years before their clinical onset.
This demonstrates that chronic fatigue is not just a feeling, but a measurable contributor to neuro-degenerative risk. Critically, the focus must shift to sleep architecture—the quality of specific sleep stages.
New research reveals that lower proportions of time spent in Slow Wave Sleep (SWS) and Rapid Eye Movement (REM) sleep are associated with reduced brain volume in regions like the inferior parietal area, which is known to undergo early structural changes in Alzheimer's disease.
This link suggests that insufficient neuroactivity during sleep may contribute to brain atrophy, fundamentally increasing the risk of Alzheimer’s disease pathogenesis and cognitive impairment. The overall dementia risk, based on specific markers, increases by 33% due to chronic sleep debt.
Immune System Failure

Sleep plays a vital role in maintaining immune function. When a person is chronically sleep-deprived, the body’s natural defenses against infections cannot function optimally. Specifically, the activity of natural killer cells, which are essential immunity protectors, becomes less active.
This suppressed immune state means individuals are approximately three times more likely to catch a cold. Beyond acute illness, long-term sleep loss is also associated with more serious medical conditions, including a 36% increased risk for colorectal cancer.
This collective evidence firmly establishes that sleep is the foundation of a robust defense against illness, infection, and even serious malignancy.
The Recovery Roadmap: Actionable Steps for 2025
The pivot from profound health destruction back to stable wellness requires acknowledging that traditional, quick-fix solutions often fail. Many individuals try restrictive diets, intense exercise regimes, or over-the-counter supplements without addressing the root problem of sleep disruption.
Furthermore, clinical experience shows that sleep-inducing medications have not been found to be as effective as behavioral therapies for chronic insomnia.
This is because medication typically only treats the symptoms, whereas behavioral therapies address the underlying cognitive and behavioral factors that initiate and maintain insomnia symptoms.
The Gold Standard: Cognitive Behavioral Therapy for Insomnia (CBT-I)

The most effective, evidence-backed treatment for chronic sleep disorder is Cognitive Behavioral Therapy for Insomnia, widely known as CBT-I. This is not a single technique but a multi-component intervention that comprehensively targets the negative behavioral and cognitive patterns surrounding sleep.
Modern therapeutic approaches emphasize specific language to improve patient engagement and compliance.
Experts recommend using the term "Sleep Efficiency Training" instead of the older term "sleep restriction" because the latter often causes anxiety and may lead patients to decline treatment. The focus is on quality and efficiency, not deprivation.
CBT-I protocols are typically comprised of four core components that work together to restore the body’s natural ability to sleep.
The Four Pillars of Sleep Efficiency Training
✨ The 4 Pillars of Sleep Efficiency Training (CBT-I) ✨
Focus on **Quality** over quantity of time spent in bed.
The Core Stat: Calculate the actual time you're asleep vs. time in bed. Gradually increase time in bed *only* as sleep improves.
Goal: Consolidate sleep and reduce fragmented rest.
Break the association between your bed and **wakefulness/frustration**.
The Rule: The **"20-Minute Rule."** If you are awake for more than 20 minutes (or worried about it), *leave* the bed.
Action: Only return when you feel distinctly sleepy. The bed is for sleep and sex, only.
Techniques to manage the **"racing mind"** and sleep-related anxiety.
Key Technique: **Reframing** negative thoughts about sleep failure ("I'll never sleep") into balanced ones ("I'll be tired, but I can still cope").
Tip: Schedule a 15-minute "Worry Time" earlier in the evening, far away from bedtime.
Rigidly maintain a consistent **WAKE-UP TIME** every single day.
Consistency Stat: A consistent wake-up time is the single most important factor for regulating your **Circadian Rhythm** (internal clock).
Avoid: Heavy meals, caffeine, and screens close to bedtime.
1. Sleep Efficiency Training (SET)

This component, formerly known as Sleep Restriction Therapy (SRT), is designed to increase the homeostatic sleep drive—the pressure to sleep that builds up when awake.
The treatment involves initially limiting the time spent in bed to closely match the actual time spent asleep. For example, if a patient is only sleeping five hours but spending eight hours in bed, the initial time allowed in bed might be restricted to five and a half hours.
As sleep consolidation improves, the time in bed is gradually increased. This strategic reduction strengthens the link between the bed and effective sleep.
2. Stimulus Control Therapy (SCT)
Stimulus control is crucial for breaking the negative psychological association between the bedroom and wakefulness, stress, or anxiety. The fundamental goal is to strengthen the bed and bedroom as cues signaling to the brain that it is time to sleep.
The primary action rule is clear: dedicate the bedroom only to sleep and sex. If sleep does not occur within approximately 20 minutes of going to bed, the individual must leave the bedroom and engage in a relaxing activity, such as reading or listening to soothing music.
They should return to bed only when they feel sleepy, repeating the process as necessary, while rigidly maintaining their scheduled wake-up time.
3. Cognitive Therapy (CT)
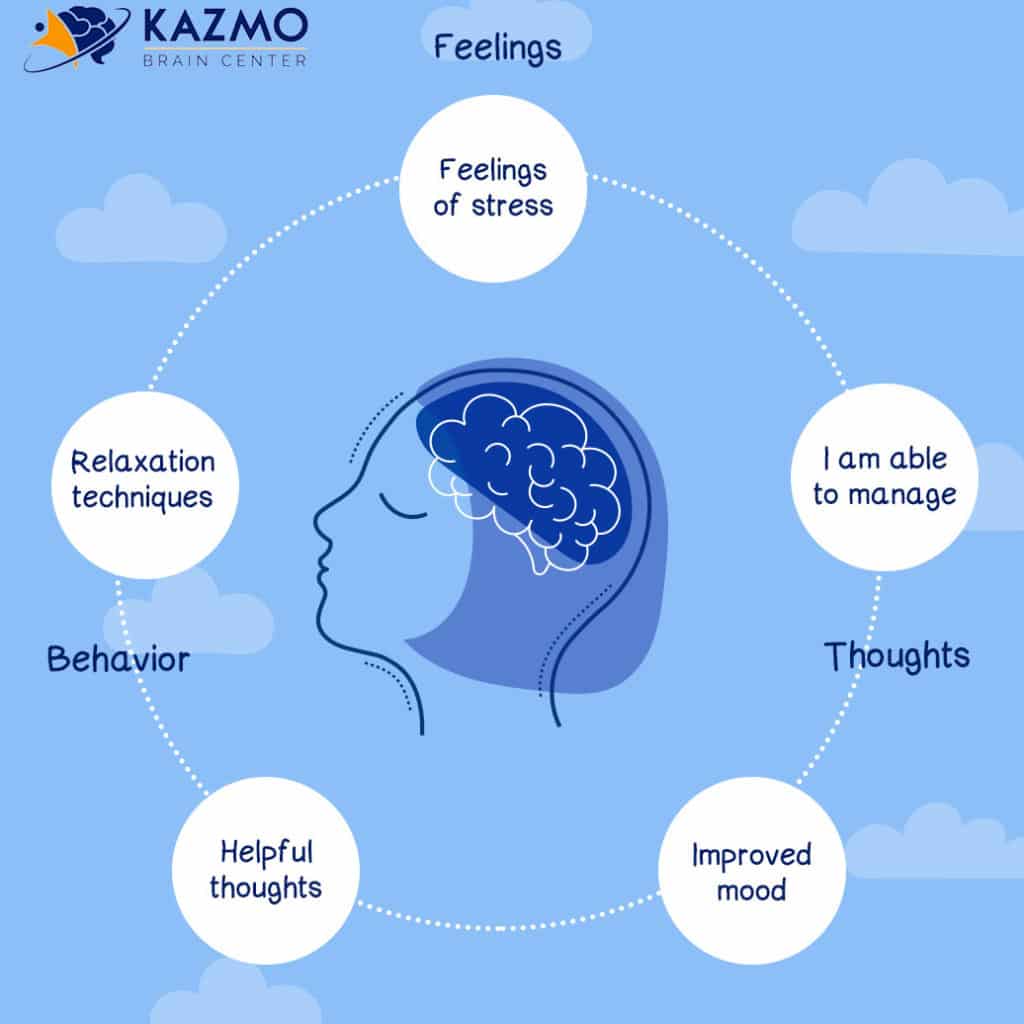
This component addresses the anxious and catastrophic thoughts and beliefs that frequently sabotage sleep. Individuals in recovery learn techniques to help them relax at bedtime and methods to reframe unhelpful thought patterns.
This often involves guided breathing, meditation, and other relaxation techniques designed to quiet a racing mind and foster emotional self-regulation.
4. Sleep Hygiene (SH)

Sleep hygiene involves establishing the foundational habits necessary for sustaining long-term sleep health. The most critical factor is consistency: maintaining the same bedtime and wake-up time every single day, including weekends, to reinforce the body’s natural sleep-wake cycle.
The sleeping environment must be optimized, prioritizing a space that is cool, dark, and quiet. Avoiding prolonged use of light-emitting screens just before bedtime is essential, as the light exposure interferes with the body’s natural sleep cues.
Furthermore, dietary habits require adjustment; large or heavy meals should be avoided within a couple of hours of sleep, and stimulating substances like nicotine and caffeine must be limited.
Even though alcohol may initially induce sleepiness, it consistently disrupts the quality of sleep later in the night and should be avoided.
Leveraging 2025 Technology for Optimization
For the modern individual seeking recovery, technology offers powerful tools to enhance CBT-I compliance and provide critical data on sleep architecture—the quality of SWS and REM that is vital for brain health.
Wearable and Non-Wearable Trackers

To move beyond simple duration measurement and focus on sleep quality, tracking internal metrics like sleep stages, heart rate variability (HRV), and oxygen levels is recommended.
Expert-recommended wearable devices provide the most detailed picture of recovery. Top choices often include the Oura Ring 4 (recognized as a best overall option) and the WHOOP 4.0 (highly rated for active users).
For those who prefer non-wearable options, the Withings Sleep mat offers effective monitoring by tracking metrics from beneath the mattress. Using these technologies allows the individual to objectively monitor the improvement in deep, restorative sleep necessary for cellular repair and cognitive restoration.
Digital CBT-I and Relaxation Apps

Digital health platforms have made clinical-grade behavioral interventions widely accessible and cost-effective. Apps rooted in CBT-I protocols, such as Chorus Sleep and Stellar Sleep, provide structured, self-guided sessions that address the cognitive and behavioral factors maintaining insomnia.
For managing the emotional and cognitive aspects of sleep disruption, dedicated meditation apps like Calm and Headspace offer guided relaxation, breathing exercises, and techniques specifically designed to quiet the mind before bed.
These tools provide accessible, continuous support, making the gold standard of care available outside of a clinical setting.
A Life Restored: The Long-Term Commitment and Longevity

The journey of recovery from chronic sleep debt is often characterized by initial difficulty, but the prognosis is overwhelmingly positive.
While the destructive effects of severe sleep deprivation on the brain and body are severe, current scientific data suggests that these effects are largely reversible with consistent and adequate sleep restoration.
This assurance is vital for recovery, helping to transform the narrative from one of past failure to one of future capability.
Building Resilience Through Goal Setting

Sustained recovery requires a structured, forward-looking plan. The focus must be shifted away from dwelling on past hurts or failures and concentrated instead on solving present problems and focusing on future goals.
Individuals should formalize their recovery by setting clear, written goals—both short-term, easily achievable targets, and larger, long-term objectives. These steps provide immediate validation and a sense of hope, reinforcing the commitment to change.
A critical element of this planning involves the identification and management of personal triggers—those places, circumstances, or people that consistently disrupt sleep or increase anxiety.
By clearly listing these triggers, the recovering individual can develop specific, prophylactic strategies to maintain emotional self-regulation and uphold sleep commitments.
Furthermore, the sense of isolation that often accompanies chronic illness is mitigated by building strong connections and seeking out supportive communities, fostering the communal understanding necessary for resilience.
The Ultimate Reward: Longevity and Clarity
Optimal Sleep: The Best Investment for Your Longevity 📈
Consistent, **optimal sleep** directly translates to *years* of extended life.
Longevity Stats (Starting at Age 30):
- Men gain an average of **+4.7 years**.
- Women gain an average of **+2.4 years**.
*Source: Longitudinal studies linking healthy sleep patterns to life expectancy.*
Investment isn't about time in bed, but **depth** of restorative sleep.
Key Metrics to Track:
- **Slow Wave Sleep (SWS):** Essential for **physical repair** and growth hormone release.
- **REM Sleep:** Critical for **cognitive processing**, memory consolidation, and emotional regulation.
*The goal is **7-9 hours** of sleep, rich in these stages.*
Technology helps you monitor recovery and **optimize sleep environment**.
Top Wearables for Deep Rest:
- **Oura Ring 4:** Excellent for tracking **Body Temperature** and sleep stage timing.
- **WHOOP 4.0:** Focuses heavily on **Heart Rate Variability (HRV)** as a marker of nervous system recovery.
*Use data to identify habits that lower your HRV and reduce deep sleep.*
The final motivation for prioritizing sleep lies in its profound impact on life span and quality. Consistent, optimal sleep—defined as maintaining the recommended 7 to 9 hours nightly—is fundamentally protective against the systemic damage described previously.
A pivotal study examining the association between sleep quality and life expectancy revealed a substantial quantitative benefit.
For individuals aged 30 years who maintained optimal sleep patterns, the average life expectancy was 4.7 years greater for men and 2.4 years greater for women compared to those with low-quality sleep.
This correlation between high-quality sleep and extended longevity underscores the fact that sleep is not merely a mechanism for temporary rest, but a core determinant of overall health, vitality, and extended life.
By mastering the techniques of Sleep Efficiency Training and leveraging modern technology, individuals move beyond mitigating damage and begin to invest directly in their long-term health, cognitive clarity, and future years.