Bone Density Breakthrough: Stop Taking Just Calcium—You Need This “Nutrient Duo” For Stronger Bones
Taking calcium supplements for strong bones? You might be doing more harm than good, and your arteries are paying the price.
Here’s the alarming reality: 1 in 3 women and 1 in 5 men over 50 will experience osteoporotic fractures, yet studies show calcium supplement users had nearly double the risk of heart disease compared to those getting calcium from food.
In this guide, you’ll discover why calcium alone doesn’t reach your bones, the crucial “traffic cop” vitamin that directs calcium where it needs to go, evidence-based dosages that work based on research, and how to implement this approach safely for optimal bone density and cardiovascular health.
The answer lies in understanding how vitamin D and vitamin K2 work together with calcium.
The Calcium Paradox
Heart vs. Bone
Calcium supplements without direction don’t just fail your bones—they calcify your arteries. Users face nearly double the risk of heart disease.
Why Your Calcium Supplements Might Be Hurting Your Heart (And What to Add Instead)

You take calcium every day for your bones. Your doctor probably told you it would prevent fractures. But here's what nobody mentions: calcium alone can end up in your arteries instead of your bones.
More than 10 million people over 55 suffered hip fractures in 2019. The numbers keep climbing. You might think the solution is simple: take more calcium. But research from 2025 shows that's exactly the wrong approach. Taking calcium by itself misses two critical partners that tell your body where to put it.
Your bones need calcium. Your heart definitely doesn't. This guide shows you how to make sure calcium ends up in the right place. You'll learn why the trio of calcium, vitamin D3, and vitamin K2 works when calcium alone fails.
The Calcium Paradox: Why More Isn't Better

Your body can't use calcium the way you think it does. When you swallow a calcium pill, your body treats it like a delivery truck with no address. The calcium enters your bloodstream, but without the right signals, it doesn't know where to go. This causes real problems.
Osteoporosis affects 10.2% of adults over 50 right now. Experts predict that number will jump to 13.6% by 2030. You'd think taking calcium would fix this. But studies show that calcium alone doesn't reduce hip fractures at all. Neither does vitamin D by itself. Only when you combine them does fracture risk drop by 19%.
Here's where it gets concerning. When researchers tested women taking calcium supplements, 9% developed too much calcium in their blood. Another 31% had excess calcium showing up in their urine. That calcium had to come from somewhere. Instead of staying in bones where it belongs, it was floating around causing problems.
The bone loss numbers tell a scary story. If you lose just 10% of bone mass in your hip, your fracture risk jumps to 2.5 times higher. Hip fractures cost the UK healthcare system an estimated £5.5 billion per year by 2025. Each fracture changes someone's life forever. Many people never fully recover their independence.
The problem is what doctors call "calcium loading." When you take a big dose of calcium all at once, your body can't process it properly. Think of it like dumping a bucket of water on a plant instead of using a watering can.
The water runs off instead of soaking in. The same thing happens with calcium supplements. Your body absorbs what it can handle, and the rest? It ends up places you don't want it.
The Hidden Danger: Calcium in the Wrong Places
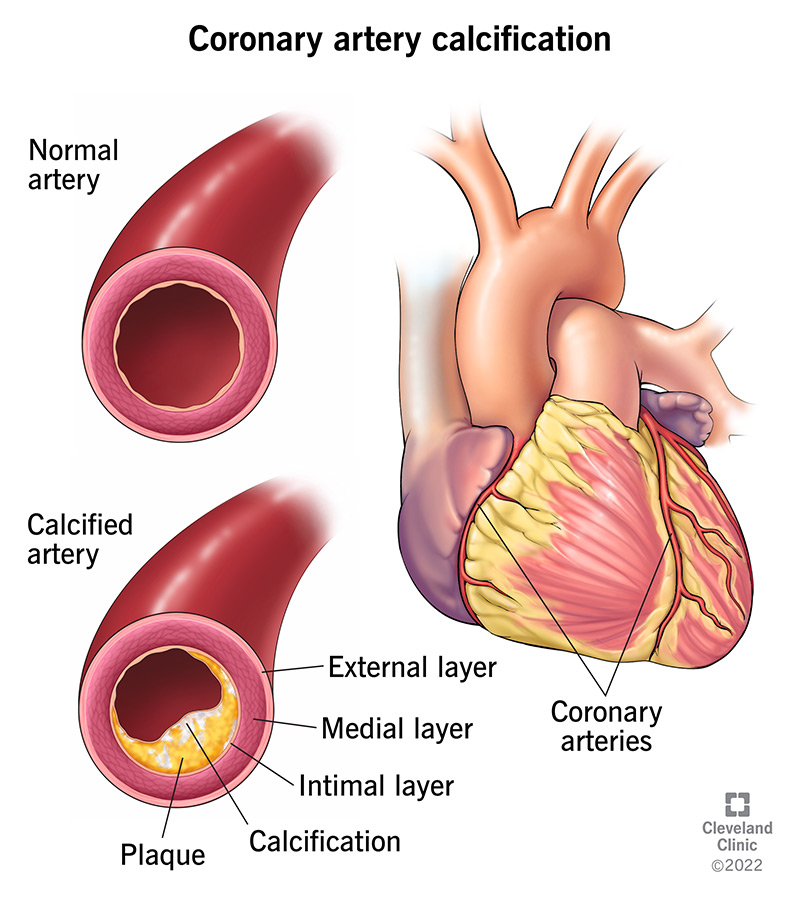
Your arteries should stay soft and flexible. But excess calcium can turn them hard and brittle. This happens when calcium deposits stick to damaged areas in your blood vessels. It's like rust forming on a scratch in metal. Once it starts, it keeps building up.
Women who took more than 1,400 mg of calcium daily from supplements faced double the risk of heart disease. Another study found that calcium supplement users had 86% higher risk of heart attacks compared to non-users.
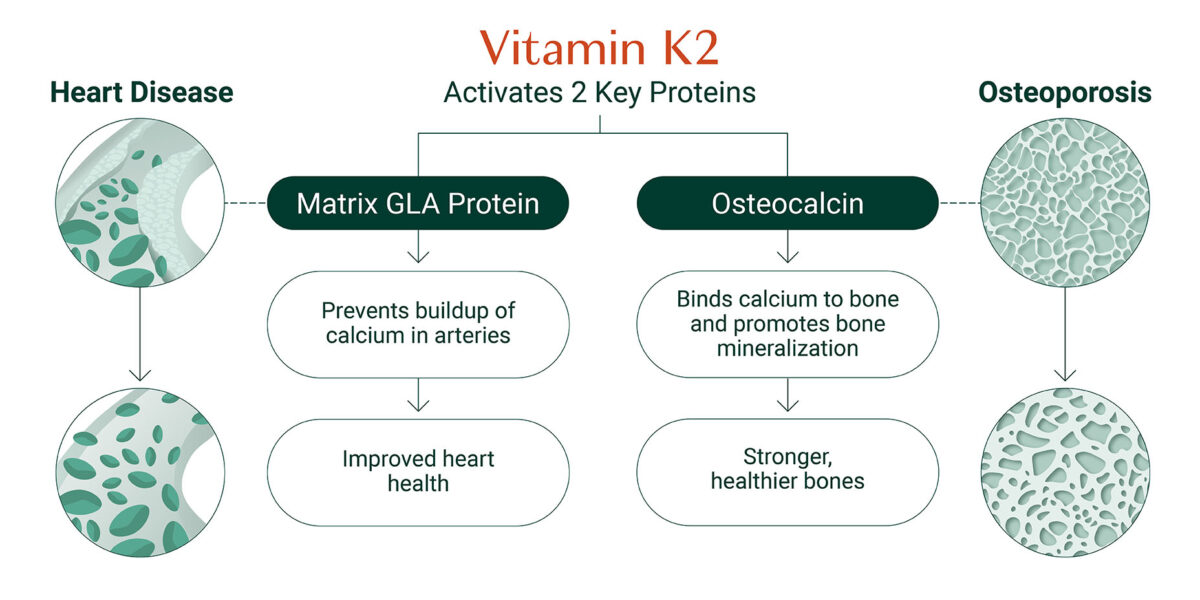
Your body has a protein called Matrix Gla-protein (MGP) that acts like a security guard. It prevents calcium from sticking to your artery walls. But MGP only works when it's activated by vitamin K2.
Doctors sometimes see something called milk alkali syndrome in people taking too many calcium supplements with antacids. Your blood becomes too alkaline. You feel nauseous, confused, and weak. In severe cases, it damages your kidneys.
Coronary artery calcium scores measure how much calcium has built up in your heart arteries. A score of zero is perfect. Anything above 100 means you have significant calcification.
Above 400 indicates very high risk for heart problems. Many people taking calcium supplements for years discover their scores climbing higher. They thought they were protecting their bones, but they were actually hardening their arteries.
Enter the Duo: How Vitamin D and K2 Work Together
Vitamin D and K2 act like a delivery team for calcium. D grabs the calcium from your food and pulls it into your bloodstream. K2 tells your body exactly where to put it. Without both working together, calcium becomes a problem instead of a solution.
Think of vitamin D as the shipping department. It increases calcium absorption from your intestines. Studies show it directly affects bone metabolism. But getting calcium into your blood is only half the job. You need K2 to complete the delivery.
Vitamin K2 activates two critical proteins: osteocalcin and Matrix Gla-protein. Osteocalcin is like a construction worker in your bones. It grabs calcium from your blood and cements it into your bone structure. But osteocalcin sits there useless until K2 activates it through a process called carboxylation.
Matrix Gla-protein (MGP) does the opposite job in your arteries. It grabs calcium before it can stick to artery walls and escorts it away. But just like osteocalcin, MGP needs K2 to activate it. Without K2, both proteins sit idle. Calcium builds up in your arteries while your bones stay weak.
Research on osteoporotic patients getting surgery showed better outcomes when they took combined K2 and D3 therapy. Another study found that vitamin K combined with calcium increased lumbar spine bone density significantly more than calcium alone. The standardized mean difference was 0.20, which means real, measurable improvement.
Postmenopausal women taking 90 micrograms of K2 daily showed significantly reduced bone loss. Their bones stayed denser compared to women not taking K2. The effect was clear and consistent across multiple studies. This wasn't a small benefit. It was the difference between maintaining bone strength and slowly losing it year after year.
The carboxylation process sounds complicated, but it's actually simple. K2 adds a chemical group to proteins that changes their shape. This shape change allows them to grab onto calcium molecules. Without this activation step, the proteins can't do their jobs. It's like having a lock but no key.
The Science Behind Vitamin K2: MK-7 vs MK-4
Not all vitamin K2 is created equal. The form called MK-7 stays in your bloodstream much longer than MK-4. This matters because consistent levels work better than spikes and crashes. Your body can use MK-7 throughout the day, not just for a few hours after you take it.
MK-7 has higher bioavailability than other vitamin K forms. Your body absorbs it better and keeps it active longer. Studies using 100 to 180 micrograms of MK-7 daily showed improved osteocalcin carboxylation and reduced bone loss. These doses are achievable and safe for most people.
MK-4 has a half-life of only one hour. MK-7 stays active for about 72 hours. If you miss a dose of MK-7, you're still covered. Miss a dose of MK-4, and your levels drop immediately. This makes MK-7 more forgiving and easier to maintain consistent levels.
Food sources for K2 are limited but powerful. Natto, a fermented soybean dish from Japan, contains 775 to 1,765 micrograms per 100 grams. That's more than any other food source by far. Egg yolks from pasture-raised chickens contain some K2. Grass-fed dairy products like cheese and butter have small amounts.
Natto is the rock star of K2 sources, but most people outside Japan find the taste challenging. The texture is slimy and sticky. The smell is strong. If you can handle it, a small serving gives you all the K2 you need. If not, supplements are a practical alternative.
Real Results: What the 2025 Research Shows
The evidence keeps getting stronger. A 2025 meta-analysis in Frontiers in Endocrinology examined vitamin K2 and bone turnover markers. The results showed clear benefits for bone health.
A three-year study on low-dose MK-7 supplementation showed something remarkable. Age-related bone density decline significantly decreased in the supplement group. They didn't just slow bone loss. They nearly stopped it. Their bones at year three looked almost as dense as at the start.
A December 2025 study reported bone mineral density increased 41% more with vitamin D and calcium supplements compared to other interventions. That's not a small improvement. That's the difference between bones that break easily and bones that stay strong.
The Multi-Ethnic Study of Atherosclerosis (MESA) tracked thousands of people for years. Those with higher vitamin K intake showed less arterial calcification. The Rotterdam Study found similar cardiovascular benefits. People eating more K2-rich foods had lower rates of heart disease and lived longer.
Chinese studies on postmenopausal women showed consistent results. Women taking the calcium, D3, and K2 combination maintained better bone density than those taking only one or two of these nutrients. The effect was measurable, predictable, and repeated across different populations.
Bone density numbers matter, but actual broken bones matter more. Studies tracking fracture rates found 15% to 25% fewer fractures in people taking the full trio compared to calcium alone. That translates to fewer hospital visits, fewer surgeries, and better quality of life in older age.
Your Action Plan: Getting the Trio Right

Start with calcium from food whenever possible. Dairy products, leafy greens, sardines with bones, and fortified foods give you calcium slowly throughout the day. If you can't get 1,000 to 1,200 mg daily from food, add a supplement to make up the difference. But always count your food sources first.
Vitamin D3 should be 800 to 1,000 IU daily for most adults. Your goal is blood levels above 30 ng/mL, ideally between 40 and 60. You can't guess your levels. You need a blood test called 25(OH)D to know where you stand. Many people are surprised to discover they're deficient even while taking supplements.
Vitamin K2 in the MK-7 form at 100 to 180 micrograms daily supports bone health effectively. Start with 100 mcg if you're new to K2 supplements. You can increase to 180 mcg after a few weeks if needed. These doses are safe for most people without blood clotting disorders or warfarin therapy.
Timing matters for absorption. Take all three with a meal that contains some fat. Vitamins D and K2 are fat-soluble. They need dietary fat present to absorb properly. A handful of nuts, some avocado, or cooking oil in your meal provides enough fat. You don't need a huge amount.
If you take calcium supplements, split the dose. Your body absorbs calcium best in amounts of 500 to 600 mg or less. Taking 1,200 mg all at once means much of it passes through unused. Take 500 mg with breakfast and 500 mg with dinner for better absorption.
Testing gives you real information instead of guesses. Ask your doctor for a 25(OH)D vitamin D test at your next checkup. If you're over 50 or have risk factors for osteoporosis, request a bone density scan called a DEXA scan. These tests show exactly where you stand.
Food sources simplify the whole process. Greek yogurt gives you calcium and some D. Sardines provide calcium and D. Natto or aged cheese adds K2. One egg yolk contains small amounts of all three. Building meals around these foods reduces how many pills you need to take.
Consistency beats perfection. Taking your supplements most days works better than taking huge doses occasionally. Your body uses these nutrients continuously. Steady supply produces better results than sporadic megadoses. Set a phone reminder if you tend to forget.
Who Should NOT Take This Combo: Important Warnings
Warfarin users must avoid vitamin K2 supplements completely. Warfarin works by blocking vitamin K. Taking K2 supplements interferes with warfarin's effectiveness. Your blood clotting could become unpredictable and dangerous. If you take warfarin, this supplement combination is not safe for you.
Kidney disease patients have trouble processing calcium. Their kidneys can't remove excess calcium properly. Taking calcium supplements can cause dangerous buildups. If you have any kidney problems, talk to your nephrologist before considering calcium supplements. The risks outweigh potential benefits.
People with hypercalcemia already have too much calcium in their blood. Adding more through supplements makes the condition worse. Symptoms include nausea, confusion, extreme thirst, and frequent urination. Causes vary from overactive parathyroid glands to certain cancers.
Active blood clotting disorders require medical supervision. Vitamin K affects how your blood clots. Some people have conditions where their blood clots too easily. Others have disorders where clotting doesn't work properly. Either way, vitamin K supplementation needs doctor oversight.
Several medications interact with this nutrient trio. Proton pump inhibitors reduce calcium absorption. Taking them long-term increases osteoporosis risk, yet adding calcium supplements might not help as much as expected. Anticonvulsant medications affect vitamin D metabolism.
Signs of calcium overload include constipation, kidney stones, nausea, and fatigue. If you experience these while taking calcium supplements, stop and see your doctor. Blood work can check your calcium levels. Too much calcium in your blood damages your kidneys and heart over time.
Get blood work before starting supplements if you're unsure about your status. A basic metabolic panel checks calcium levels. Adding a 25(OH)D test for vitamin D gives you a complete picture. These simple tests prevent problems before they start. Insurance usually covers them as part of routine care.
Pregnancy and breastfeeding change your nutrient needs. While calcium and vitamin D are important during these times, doses need adjustment. Vitamin K2 research during pregnancy is limited. Always consult your obstetrician before taking any supplements while pregnant or nursing.
Common Mistakes That Waste Money
Taking calcium carbonate without food is pointless. Your stomach needs acid to break down this form of calcium. Food triggers acid production. On an empty stomach, the calcium carbonate just passes through unabsorbed. You literally flush money down the toilet. If you use calcium carbonate, always take it with meals.
Megadoses of calcium over 2,500 mg daily cause problems without extra benefits. Your body can't use that much. The excess increases your risk of kidney stones and arterial calcification. More is not better with calcium. Stick to 1,000 to 1,200 mg total from all sources.
You increase calcium absorption but don't direct where it goes. This might actually increase arterial calcification while failing to strengthen bones properly. The duo works together. Taking only one wastes the potential of both.
K2 doses under 100 micrograms probably won't affect your bones much. Research showing benefits used at least 90 to 100 mcg daily. Lower doses might support general health but won't provide the bone protection you're looking for. Don't waste money on underdosed K2 supplements.
Ignoring dietary sources means taking more pills than necessary. A cup of yogurt gives you 300 mg of calcium. Three ounces of sardines provide another 325 mg plus vitamin D. You might only need a 500 mg calcium supplement instead of 1,200 mg if you count your food. Less supplementation usually means fewer side effects.
Buying low-quality supplements saves money upfront but costs you in the long run. Some brands don't contain what their labels claim. Others use forms that absorb poorly. Third-party testing from USP, NSF, or ConsumerLab verifies quality. Look for these symbols on bottles. They confirm you're getting what you pay for.
Buying vitamin K1 instead of K2 is a common error. K1 supports blood clotting. K2 supports bone and heart health. They're different vitamins with different jobs. Check your supplement label carefully. It should say "vitamin K2" or "menaquinone," specifically "MK-7" for best results.
Poor timing reduces absorption significantly. Taking fat-soluble vitamins like D and K2 with a fat-free meal means your body absorbs only a fraction. Taking calcium in huge single doses instead of split doses cuts absorption in half. These timing mistakes mean you absorb maybe 30% to 40% of what you paid for.
Your Bones Need a Team Approach
Calcium alone is insufficient and potentially harmful. Research from 2025 proves this beyond doubt. When calcium floats around your bloodstream without direction, it ends up in your arteries instead of your bones. The damage accumulates slowly over years until you face serious cardiovascular problems.
The D3 and K2 duo ensures calcium reaches bones, not arteries. Vitamin D pulls calcium from your food into your blood. Vitamin K2 activates the proteins that cement calcium into bone and keep it out of arteries. This three-way partnership works better than any single nutrient alone.
Evidence from multiple 2025 studies supports this approach. Women taking the combination showed 41% greater bone mineral density improvement. Fracture rates dropped 15% to 25%. Arterial calcification progressed more slowly. These aren't theoretical benefits. They're real outcomes in real people.
Your dosage starting point: 1,000 to 1,200 mg calcium (primarily from food), 800 to 1,000 IU vitamin D3, and 100 to 180 mcg vitamin K2 MK-7. Take them with a fat-containing meal. Split calcium doses if supplementing. Get blood work to check your vitamin D levels after three months.
Before your next calcium supplement purchase, talk to your healthcare provider about adding vitamin D3 and K2 to your regimen. Your bones and your heart will thank you. The research is clear. The combination works. The only question is whether you'll use this information to protect your health.