The “Mouth Microbiome” Secret: Why Brushing Your Teeth Isn’t Enough To Prevent Heart Disease
Your dentist has been telling you something crucial about your heart health, but you might not have been listening. Every time you skip flossing, harmful bacteria travel through your bloodstream, potentially contributing to the leading cause of death in America.
While you brush twice daily, standard brushing removes only 40 to 60 percent of plaque, leaving dangerous bacteria that trigger systemic inflammation and oral microbiome heart disease.
A 2024 review shows interdental cleaning significantly lowers periodontitis and cardiovascular disease mortality. You will learn how oral bacteria inflammation impacts gum disease heart attack risk, exploring scientific mechanisms and evidence-based strategies to reduce cardiovascular risk by 43 percent.

The Oral-Heart Connection: Why Your Dentist Might Save Your Life
The Secret Invasion
THE SNEAK ATTACK
You brush twice a day, but germs hide in the “back alleys” between teeth. Brushing misses 40-60% of the surface!
You brush twice a day. You think you're doing everything right. But your gums bleed when you floss, and you've been putting off that dentist appointment for months. What if I told you that bleeding could be connected to your heart health?
Recent research shows something surprising: the bacteria in your mouth don't stay in your mouth. They travel. And where they go matters more than you might think.
How Mouth Bacteria Reach Your Heart
Here's what scientists found in 2024. They looked at samples from people with heart disease. What they discovered was shocking. They found 410 types of oral bacteria in gut samples.
They found 221 in blood samples. And they found 169 in the plaques blocking arteries. Think about that. Bacteria from your mouth, living in your arteries.
How do they get there?
Every time you chew food, your gums flex and move. If your gums are inflamed (swollen and irritated), tiny openings form. Bacteria slip through these openings into your bloodstream. Even brushing can cause this if your gums aren't healthy.
Three specific bacteria show up again and again in heart disease patients: P. gingivalis, F. nucleatum, and A. actinomycetemcomitans. Remember these names. They're not your friends.
Three ways bacteria travel from the mouth to the heart:
First, they enter directly through damaged gum tissue. This happens daily if you have gum disease.
Second, you swallow them. A 2024 study showed that oral bacteria travel to your gut and change the balance of bacteria there. Your gut health then affects your heart through what scientists call the oral-gut-heart axis.
Third, they trigger inflammation. Bacterial toxins from your mouth cause your body to release inflammatory chemicals. These chemicals travel through your whole system and promote the buildup of plaque in your arteries.
The inflammation link is critical.
When you have poor oral hygiene, your C-reactive protein (CRP) goes up. CRP is a marker of inflammation in your body. High CRP levels are linked to heart disease.
Here's the scale of the problem: Heart disease kills 17.9 million people worldwide every year. Gum disease (periodontitis) is the sixth most common disease on the planet. Your mouth and your heart are more connected than you ever imagined.
The Numbers Tell a Scary Story

Let's talk statistics. Real numbers from real studies. People with gum disease are 1.5 to 2.8 times more likely to develop heart disease or have a stroke. That's not a small increase. That's huge.
About half of American adults over 30 have some level of gum disease. Almost 10% have severe disease.
Here's what surprised researchers: younger patients under 45 with gum disease show worse outcomes. In this group, 23.8% have heart disease. Compare that to only 7.5% of older patients with similar gum problems.
The American Heart Association noticed.
In December 2025, they released a new scientific statement. They said the evidence keeps growing. Gum disease is linked to heart attack, stroke, irregular heartbeat, and heart failure.
This connection exists even when researchers account for other risk factors. Smoking, diabetes, and obesity—they controlled for all of these. The link between gum disease and heart problems remained.
They haven't proven that gum disease causes heart disease. But the biological mechanisms make sense. The evidence keeps piling up.
Breaking down the numbers in heart disease patients with gum disease:
- 25.3% have high blood pressure
- 6.6% have coronary heart disease
- 1% have had a stroke
- 1.1% have heart failure
Regional differences matter too. Americans have a 13.3% heart disease. Europeans have 12%. Asians have 8.2%.
Imagine two 62-year-olds. Same diet, same exercise habits, same family history. One has severe gum disease. One has healthy gums. Their risk for heart problems is dramatically different. Your oral health is a heart disease risk factor. Period.
Why Your Toothbrush Isn't Enough

You brush for two minutes twice a day. Good. But it's not enough. Research from the UAB School of Dentistry shows that brushing removes only 40% to 60% of plaque. Where does the other 40-60% hide? Between your teeth.
Your toothbrush can't reach these spaces. The bristles are too thick. The gaps are too narrow.
Think of your mouth as a city.
The surfaces of your teeth are like main streets. Easy to clean. Your toothbrush handles these well.
But between your teeth? Those are the back alleys. Dark. Hidden. That's where bacteria set up camp.
These bacteria don't live alone. They form communities called biofilms. Picture a tiny city with walls, communication systems, and protection. Your toothbrush hits the surface of this city but leaves the colony intact.
Here's what most people get wrong about oral bacteria.
You have over 700 species of bacteria in your mouth. The goal isn't to kill them all. That's impossible and actually harmful.
Some bacteria are good. S. salivarius, for example, produces chemicals that fight the harmful species. It's like having guards protecting your mouth.
When you use harsh mouthwashes that kill everything, you wipe out the good bacteria too. You leave a space. Often, the bad bacteria come back first and stronger. The goal is balance. Diversity. A healthy ecosystem.
Your mouth is unique.
Your oral microbiome is as unique as your fingerprint. Your genes, diet, stress levels, and medications all shape which bacteria live in your mouth.
This is why the same oral care routine works differently for different people. What keeps your sister's gums healthy might not work for you.
A 2024 study identified the three bacteria most associated with heart disease: P. gingivalis, F. nucleatum, and A. actinomycetemcomitans. All three love to hide between teeth where brushing can't reach them.
Brushing your teeth without cleaning between them is like washing the front of your car but never cleaning between the seats. You're missing the problem areas.
Flossing Changes Everything

For years, people debated whether flossing really matters. The debate is over. New research from 2024 and 2025 makes the answer clear. Flossing works. And it works better than anyone expected.
The breakthrough study came in November 2024.
Researchers looked at 18,801 adults. They tracked their habits and health outcomes. What they found was remarkable.
People who flossed daily had 29% lower rates of heart attacks and strokes. Even more impressive: they had a 36% lower risk of dying from heart disease.
That's more than one-third reduction in heart disease deaths. From flossing. A February 2025 study pushed this further. Flossing just 3-4 days per week reduced heart disease risk by 43%.
For people who already have heart disease, cleaning between teeth reduced their risk of new heart problems by 80%.
Why does flossing work so well?
Remember those back alleys where bacteria hide? Floss reaches them. It removes the bacterial colonies before they can enter your bloodstream.
This reduces inflammation. When researchers measured CRP levels (that inflammation marker we talked about), flossing brought them down significantly.
A 2025 stroke study found flossing lowers the risk of one specific type of stroke—cardioembolic stroke—by 44%. This is the kind caused by blood clots that travel to the brain. The connection to oral bacteria is direct.
Here's the longevity data.
A Finnish study tracked people for years. Those who both brushed and flossed lived significantly longer than those who only brushed.
UAB research found that people who floss daily live an average of 6.5 years longer than those who don't. Six and a half years. From flossing.
For each additional day per week that you floss, your risk of dying from heart disease drops by 6%.
Making it practical:
Traditional floss works. But it's not your only option. Interdental brushes (tiny brushes that fit between teeth) work great if you have space between your teeth. Many people find them easier to use than string floss.
Water flossers shoot a stream of water between teeth. They work well for people with braces, bridges, implants, or sensitive gums. The best tool is the one you'll actually use.
When should you floss?
Evening is ideal. You remove all the bacteria that accumulated during the day. This prevents them from sitting between your teeth all night.
How long does it take to make it a habit? Research shows 2-3 months. Set a phone reminder. Put the floss next to something you use every night. Build the habit slowly.
The data is clear: not flossing versus flossing daily means 36% higher risk of dying from heart disease. Your heart health is between your teeth.
The Mouth-Gut-Heart Highway
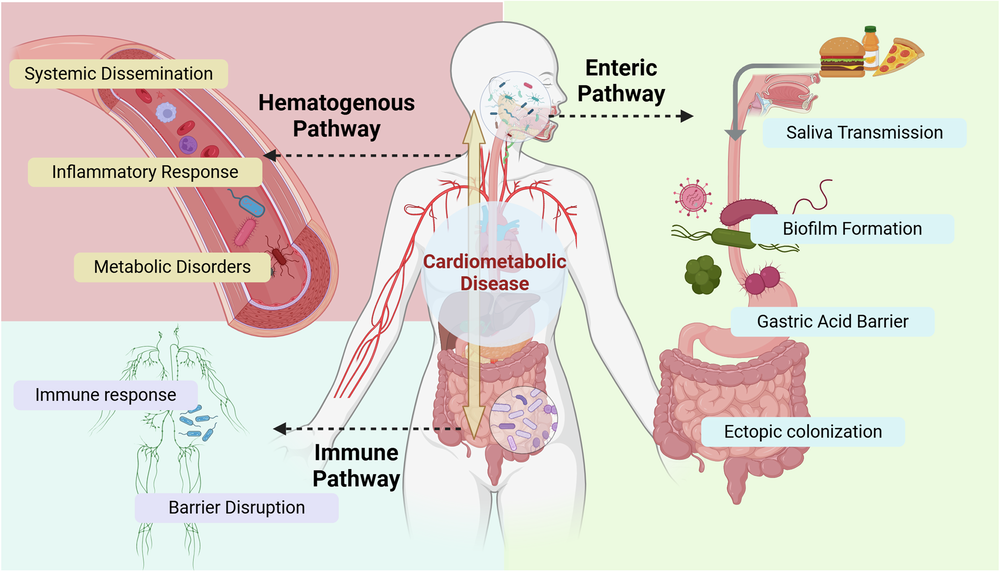
Your mouth connects to your gut. Your gut connects to your heart. It's a three-way highway. Every time you swallow, you send oral bacteria to your digestive system. This happens all day long.
An April 2024 study looked at people with diabetes and heart disease. Researchers found that oral bacteria traveling to the gut significantly affects how heart disease progresses.
January 2025 research confirmed that the oral-gut connection is critical for understanding heart and metabolic diseases.
What happens when oral bacteria reach your gut?
They change the balance of bacteria living there. Scientists gave mice an oral bacterium called P. gingivalis. This bacterium altered the ratios of two major bacterial groups in the gut: Bacteroidetes and Firmicutes.
These ratios matter. They're different in people with heart disease compared to healthy people.
Changes in gut bacteria affect what chemicals they produce. Some of these chemicals influence your blood pressure, cholesterol, and inflammation levels.
The metabolite connection:
Gut bacteria create compounds as they digest your food. Some of these compounds are good for you. Short-chain fatty acids (SCFAs), for example, help regulate inflammation and support heart health.
Other compounds cause problems. Trimethylamine N-oxide (TMAO) is one. High TMAO levels are linked to atherosclerosis (plaque buildup in arteries).
Here's the timeline:
Bacteria travel from your mouth to your gut within hours. Within 24-48 hours, they start affecting your gut bacterial balance. These changes then produce metabolites that reach your heart through your bloodstream.
The clinical implications are huge.
Treating your oral health might improve your gut health. Treating your gut health might help your oral health. They're connected.
Probiotic supplements and foods target both systems. Dietary choices affect both microbiomes at the same time. If you fix the problem at one point in the highway, you might prevent problems down the road.
Your mouth isn't isolated from the rest of your body. It's the starting point of a complex system that reaches your heart.
Beyond Flossing: Building a Complete Strategy

The December 2024 American Heart Association statement emphasized regular dental cleanings as part of heart disease prevention. Not just for healthy teeth—for a healthy heart.
Professional cleanings remove calcified plaque. This is hardened plaque that your toothbrush and floss can't remove. It requires special tools.
Dentists and hygienists also check for early signs of gum disease. Catching it early makes treatment easier and more effective.
How often? Every 6 months minimum. If you're at high risk (diabetes, family history of heart disease, smoking history), every 3-4 months is better.
Your diet shapes your oral microbiome.
Probiotic-rich foods feed the good bacteria: yogurt, kefir, sauerkraut, kimchi. These foods introduce beneficial bacteria to your system. Prebiotic fiber feeds the bacteria already there. Think vegetables, whole grains, beans.
Polyphenols in green tea and berries have natural antimicrobial properties. They help keep harmful bacteria in check.
Sugar and refined carbs? They feed the bacteria you don't want. Every time you eat sugar, you're feeding P. gingivalis and its friends.
Omega-3 fatty acids (found in fish, walnuts, flaxseeds) reduce inflammation throughout your body, including your mouth.
Oral probiotics are emerging as a tool.
This is newer science, but it's promising. A November 2024 study used engineered probiotics that produce short-chain fatty acids. These probiotics prevented heart damage in mice.
2025 research shows that specific strains of Lactobacillus and Bifidobacterium reduce inflammation markers and cholesterol levels.
One strain, Lactobacillus reuteri, produces a compound called GABA. This showed promise in reducing heart inflammation and damage.
Not all probiotics are the same. Strains that help your gut might not help your mouth. Look for probiotics specifically researched for oral health.
Lifestyle factors you might not think about:

Stress hurts your oral health. It reduces saliva production. Saliva is your mouth's natural defense system. Less saliva means more bacterial growth.
Sleep matters too. Seven to nine hours supports both oral and heart health. Poor sleep weakens your immune system's ability to fight bacteria.
Water keeps your mouth clean. It washes away food particles and bacteria. It keeps saliva flowing. Dehydration reduces saliva production.
Smoking and vaping dramatically alter your oral microbiome. They kill beneficial bacteria and allow harmful bacteria to thrive. If you smoke, quitting is the single best thing you can do for your oral and heart health.
What about mouthwash?
An 18.8-year study found that mouthwash use didn't provide additional protection against heart disease death beyond brushing and flossing. Alcohol-based mouthwashes can harm beneficial bacteria. They create an imbalance.
If you use mouthwash, choose alcohol-free, pH-balanced options. But understand it's not a replacement for mechanical cleaning (brushing and flossing). It's a supplement at best.
Monitoring your oral health:
- Bleeding gums when you brush or floss
- Bad breath that doesn't go away
- Gums pulling away from teeth
- Sensitive teeth
- Loose teeth
Get a comprehensive periodontal examination once a year. This is different from a regular cleaning. It's a detailed assessment of gum health.
Some dentists now offer oral microbiome testing. This is cutting-edge and not widely available yet. But it might become standard in the future. Ask your doctor to check your CRP levels. This inflammation marker connects oral and heart health.
A simple daily routine:
Morning:
- Brush for 2 minutes with a soft-bristle brush
- Rinse with water
- Eat a breakfast that includes probiotic-rich food (like yogurt)
Evening:
- Floss thoroughly (take 5-10 minutes to do all spaces between teeth)
- Brush for 2 minutes
- Clean your tongue (bacteria live there, too)
- Consider a probiotic supplement if your dentist or doctor recommends it
This routine takes about 15 minutes total per day. That's less time than one episode of a TV show. For potentially six and a half extra years of life.
Warning Signs Your Mouth Is Sending

Persistent bleeding when you brush or floss isn't normal. Healthy gums don't bleed easily. Bleeding means inflammation. Inflammation means bacteria are winning.
Chronic bad breath despite good hygiene is a red flag. It suggests bacterial overgrowth or gum disease. Receding gums expose tooth roots. This increases sensitivity and infection risk. It also indicates long-term gum disease.
Loose teeth or changes in how your teeth fit together signal advanced gum disease. The bone supporting your teeth is breaking down. Frequent mouth sores or ulcers can indicate immune system problems or bacterial imbalance.
Systemic symptoms connected to oral health:
Unexplained fatigue might seem unrelated to your mouth. But chronic low-grade infection drains your energy.
Joint pain or general inflammatory symptoms can stem from oral bacteria triggering system-wide inflammation.
Digestive issues like bloating or irregular bowel movements might connect to oral bacteria changing your gut microbiome. Frequent infections suggest your immune system is overwhelmed. Fighting oral bacteria leaves fewer resources for other threats.
Who should be extra vigilant?
People with diabetes have a higher risk. Diabetes and gum disease worsen each other. If heart disease runs in your family, your oral health matters even more.
Smokers and former smokers have damaged oral microbiomes. The effects can last for years after quitting.
Adults over 45 face an increased risk for both gum disease and heart disease.
If you have metabolic syndrome (a combination of high blood pressure, high blood sugar, excess belly fat, and abnormal cholesterol), oral health is critical.
When to seek care:
Immediately: Sudden gum swelling, abscess (pus-filled bump), or severe pain.
Urgently (within a week): Persistent bleeding that doesn't improve, or rapid gum recession.
Scheduled: Annual comprehensive periodontal exam even if you feel fine.
Regular: Professional cleaning every 6 months minimum.
Don't wait for pain. Gum disease often doesn't hurt until it's advanced. By the time it hurts, significant damage has occurred. Your mouth is talking. Listen to it.
What the American Heart Association Says Now
The American Heart Association doesn't make statements lightly. They review mountains of research before releasing guidance.
In December 2025, they released an updated scientific statement on oral health and heart disease.
What they confirmed:
The evidence keeps growing. Gum disease is associated with heart attack, stroke, atrial fibrillation (irregular heartbeat), and heart failure.
This isn't a weak association. It's strong enough that they're telling doctors to pay attention. They emphasized prevention and early treatment. Catching gum disease early prevents both oral damage and potential heart effects.
They recognized periodontal disease as an independent risk factor for heart disease. This means it matters on its own, not just because people with gum disease might have other risk factors too.
What this means for you:
Your oral health should be part of your heart disease risk assessment. When you see a cardiologist, they should ask about your dental health. When you see a dentist, they should ask about your heart health.
More doctors are integrating care. Your dentist and doctor should communicate, especially if you have risk factors.
Preventive dental care is now preventive heart care. Insurance companies are starting to recognize this. Some cover more frequent dental cleanings for people at high heart disease risk.
The limitations they acknowledge:
No large-scale clinical trials have proven that treating gum disease prevents heart attacks. The research exists, but that specific trial hasn't been done yet.
Most evidence comes from observational studies. These show associations and mechanisms but don't prove direct cause and effect.
More research is needed on what specific interventions work best. Should everyone with gum disease get aggressive treatment to protect their heart? How often should cleanings happen? What's the optimal approach?
Individual responses vary. Not everyone with gum disease gets heart disease. Not everyone with heart disease has gum disease. But the connection is strong enough to take seriously.
Where research is heading:
Oral microbiome testing might become part of heart disease risk assessment. Imagine testing your oral bacteria to predict heart disease risk.
Scientists are developing targeted oral probiotics specifically for heart health.
Integration of dental and medical records is coming. Your dentist will be able to see your blood pressure, cholesterol, and diabetes status. Your doctor will see your gum disease status.
Personalized oral care based on your specific microbiome profile might become standard. Different bacteria require different approaches. The American Heart Association is saying: take your oral health seriously. It's not separate from your heart health.
Your Mouth, Your Heart, Your Choice

Let's bring this together. Your mouth and your heart are connected through bacteria, inflammation, and metabolic compounds. This isn't theory. It's proven biology.
Brushing twice daily is essential. But research confirms it's not enough. Brushing reaches only 40-60% of tooth surfaces. The other 40-60% is between your teeth.
The flossing evidence is overwhelming.
Daily flossing reduces heart disease death risk by 36%. People who floss daily live an average of 6.5 years longer. Six and a half years from a habit that takes five minutes per day.
Your oral microbiome matters as much as your gut microbiome for heart health. Maybe more, because it's the starting point. Every swallow sends bacteria from your mouth to your gut. From your gut, bacterial products reach your bloodstream and your heart.
What you can do tonight:
Commit to flossing daily for 30 days. Track it. Put a checkmark on your calendar each day you do it. It takes 2-3 months to build a new habit. Start now.
If you haven't had a comprehensive periodontal exam in the past year, schedule one. Not just a cleaning—a real assessment of your gum health.
Ask your doctor to check your CRP levels at your next physical. This inflammation marker connects oral health to heart health.
Your action plan
This week: Buy floss or interdental brushes. Try both if you're not sure which you prefer.
This month: Build the daily flossing habit. Set a reminder on your phone.
This quarter: See your dentist for a comprehensive periodontal exam.
This year: Make oral care a non-negotiable part of your health routine, just like taking medications or exercising.
The partnership approach:
Your dentist and your doctor should be partners in your preventive health strategy. Tell your dentist about your heart health concerns. Tell your doctor about your gum health.
Most doctors don't ask about dental health yet. Most dentists don't ask about heart health yet. You can connect these dots yourself until the system catches up. The oral-heart connection is real. It's measurable. And most importantly, it's modifiable.
You can't change your genetics. You can't always control your stress. You can't reverse years of poor diet overnight. But you can floss tonight.
Understanding the link between gum disease and heart disease empowers you to take action. You're not helpless. Simple daily practices—brushing, flossing, regular dental care—reduce your risk.








