The Hidden 86% Stroke Risk: How Poor Oral Health Directly Causes Brain Damage and Vascular Disease
What if a common, preventable problem found in nearly half of all adults posed a shocking, nearly doubled risk of the most devastating health crisis—a stroke? For too long, the connection between dental hygiene and brain health has been overlooked, often dismissed as separate domains of medical concern.
The prevailing belief that basic dental habits only affect the condition of one’s teeth masks a profound systemic danger. Recent, definitive research now forces a critical re-evaluation of this oversight, demonstrating that poor oral health stroke risk is significantly elevated by chronic infection.
The public health sector now recognizes that neglected dental health functions as a powerful, high-leverage risk factor for vascular catastrophe. This expert report unveils the alarming 2025 findings that link the specific combination of gum disease (periodontitis) and cavities (caries) to an 86% higher ischemic stroke risk.
The 86% Stroke Risk: New Data Linking Gum Disease and Brain Clots
The 86% Risk Factor
Summary placeholder.
CLINICAL FINDINGS:
The Landmark Study: Quantifying the Dental-Vascular Link

The critical finding regarding the profound connection between oral health status and future stroke incidence stems from a long-term, large-scale investigation known as the Atherosclerosis Risk in Communities (ARIC) study.
The results, published in October 2025 in Neurology® Open Access, the official journal of the American Academy of Neurology, tracked nearly 6,000 adults, assessing their oral health status and subsequent incidence of ischemic stroke over two decades.
This extensive longitudinal research, led by Dr. Souvik Sen, MD, MS, MPH, provided the robust, long-term data necessary to establish a clear and quantifiable association between specific oral conditions and neurological outcomes.
Participants in the study, who averaged 63 years of age and had no prior history of stroke, were carefully classified into three distinct oral health groups: those with a healthy mouth, those with periodontal disease (gum disease) only.
And those suffering from the dangerous combination of periodontal disease and dental cavities (caries). The purpose of this segmentation was to isolate the risk associated with differing severities and combinations of oral infection.
The Specific Double Threat: Periodontal Disease and Caries
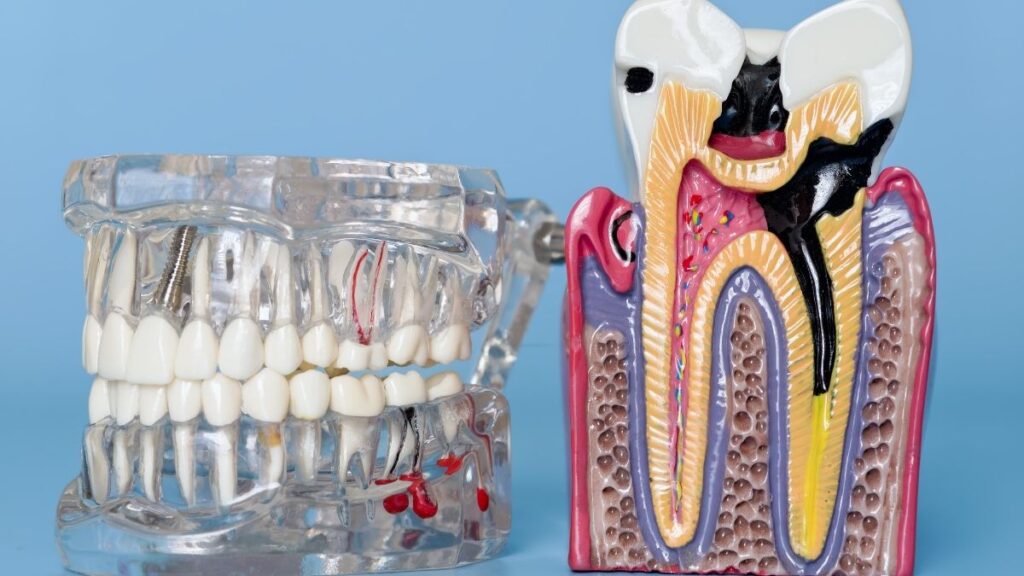
The most critical discovery confirms that the risk is not just about general dental neglect; it is about the specific synergy between gum disease and tooth decay.
The group that exhibited both gum disease stroke factors—Periodontal Disease (PD) and Caries—faced an 86% greater chance of experiencing an ischemic stroke when compared to the cohort with good oral health.
Ischemic strokes, which account for the vast majority of all strokes, occur when a blood clot or blockage restricts blood flow to the brain, leading to oxygen deprivation.
The research reinforces that while having gum disease alone carries an elevated risk, the presence of both chronic conditions creates an environment of maximized systemic danger.
The incidence of ischemic stroke across the groups starkly illustrates this risk: the healthy mouth group had a stroke incidence of 4.1%; the PD only group had an incidence of 6.9%, but the combined PD + Caries group saw their incidence rate jump to a full 10.0%.
Implications of the Combined Risk
The highly specific finding that the 86% stroke risk is tied to the combination of untreated gum disease and untreated cavities is a major insight for preventative health.
If the elevated risk were solely due to generalized inflammation, the “PD only” group would logically bear the highest burden. Instead, the data suggests that the presence of deep, chronic, untreated cavities brain damage the systemic health by contributing a unique and persistent high load of infectious agents.
Therefore, effective stroke prevention in this context requires managing both the underlying inflammation (periodontal care) and the open lesions (restorative care for caries) to eliminate the source of the systemic infection.
Beyond Gums: The Inflammation Pathway Linking Poor Oral Health to Vascular Damage
Periodontal Disease as a Leaky Barrier

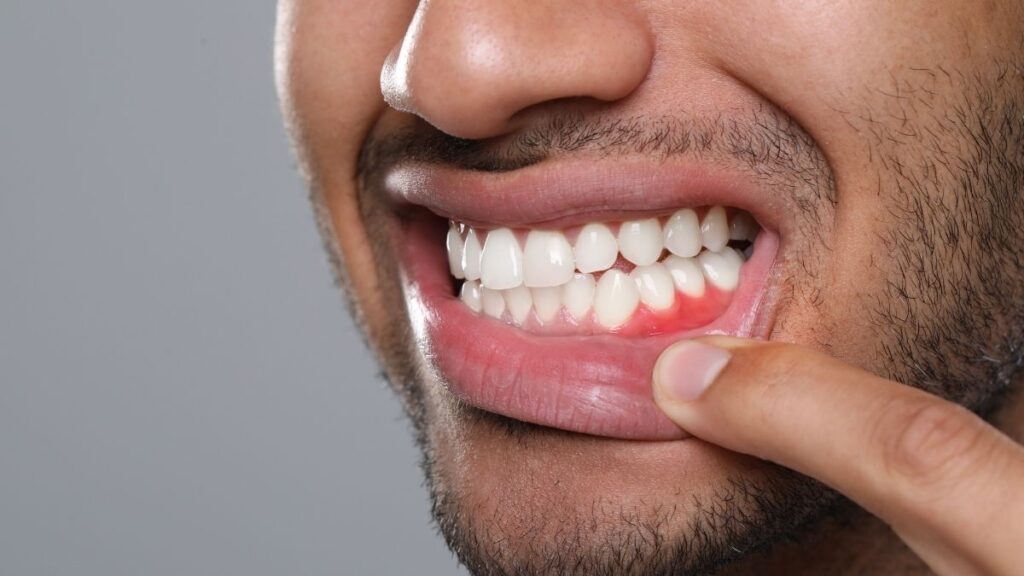
To understand how bacteria in the mouth can lead to a stroke in the brain, one must recognize periodontal disease (gum disease) not merely as a localized dental problem, but as a chronic systemic infection.
Periodontal disease is an infection and inflammation that damages the tissues supporting the teeth, creating an inflamed, leaky barrier between the mouth and the rest of the body.
This chronic infection provides a constant, open portal for oral bacteria to enter the bloodstream, a phenomenon known as bacteremia. Once in circulation, these bacterial components trigger a potent inflammatory response throughout the body.
The Systemic Fire Alarm: C-Reactive Protein (CRP)

Localized oral infections, particularly those resulting in tissue loss characteristic of periodontitis, elicit widespread systemic changes. These changes are manifested primarily by an increase in acute phase reactants, which are proteins produced by the liver in response to inflammation.
The most significant of these is C-reactive protein (CRP). CRP is widely accepted throughout the medical community as a key measure of systemic inflammation, and elevated CRP levels are strongly and consistently associated with an increased risk of atherosclerosis (the hardening and narrowing of arteries) and major cardiovascular events.
Periodontal diseases lead to a sustained increase in CRP levels in the peripheral blood. The chronic nature of the infection means the liver is constantly signaled to produce these inflammatory mediators.
In fact, patients suffering from both acute coronary syndrome (ACS) and periodontal disease have CRP levels elevated above the concentration seen with only one disease or the other, demonstrating the intense systemic burden imposed by the oral infection.
The Clotting Cascade and Vascular Acceleration
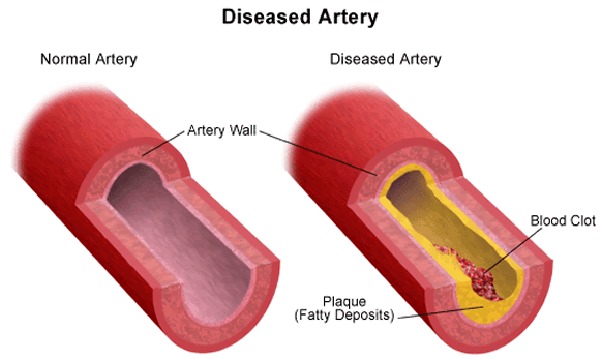
The role of CRP goes beyond being a simple diagnostic marker of inflammation; it is an active participant in vascular pathology. CRP is known to stimulate tissue factor production by monocytes (a type of white blood cell), which confers a powerful procoagulant (clot-promoting) effect on the blood.
This shift toward hypercoagulability is a primary driver of blood clot formation, which directly leads to ischemic strokes.
Furthermore, CRP contributes to the physical damage of the blood vessels themselves. It recruits monocytes via chemotaxis into the arterial wall, where it co-localizes with foam cells in atherosclerotic lesions.
This means that the inflammatory response originating from the mouth actively accelerates the buildup of plaque in the arteries throughout the body, including the carotid arteries leading to the brain.
This biological sequence explains the heightened risk found in the 2025 study for thrombotic and cardioembolic strokes, as these are precisely the types of strokes driven by clotting and atherosclerotic damage.
The combination of unchecked gum disease and open cavities’ brain damage potential is devastating because it maximizes the bacterial leakage and the subsequent inflammatory response, ensuring high, chronic CRP levels.
Your Actionable Guide to Reducing Oral Health Stroke Risk by 81%
The good news stemming from the 2025 research is that the risk, while significant, is highly modifiable. The most compelling evidence for intervention comes from data on routine professional care, which demonstrates the immense power of simple, accessible actions to mitigate the risk.
Pillar 1: Professional Care — The 81% Solution

The single most powerful preventative measure identified in the Sen study involved professional dental intervention. Individuals who utilized regular dental care were found to be 81% less likely to have the specific, high-risk combination of periodontal disease and cavities.
This statistic strongly argues that professional cleaning, scaling, and the immediate repair of open caries lesions (fillings) are the frontline defense against the 86% stroke risk.
Dental visits are not merely maintenance; they are critical preventative screenings for vascular health. A dentist can accurately screen for asymptomatic periodontal disease, which affects 47.2 million U.S. adults over the age of 30, and can remove hardened plaque (calculus) deep below the gum line.
This professional removal breaks the cycle of chronic infection, fundamentally reducing the source of systemic inflammation. Since PD is often silent in its early stages, individuals are encouraged to seek regular screenings to catch the disease early and eliminate the infectious source before the inflammatory cascade fully develops.
Pillar 2: Daily Hygiene Foundation — The Two-Minute Rule

Consistent daily oral care is the foundation upon which professional treatment builds. The American Dental Association (ADA) provides clear, evidence-based guidelines for effective home care, centered around two core activities: brushing and interdental cleaning.
Brushing for Brain Health

The ADA recommends brushing teeth twice a day with fluoride toothpaste for a full two minutes each time. This recommendation is crucial because it ensures sufficient time for the mechanical action of the brush to disrupt and remove the sticky, bacteria-laden plaque film.
If plaque is not removed consistently, the bacteria release acids that attack the tooth enamel, creating cavities, and the plaque calcifies into calculus, accelerating gum disease. Consistently adhering to the two-minute rule prevents the initial formation of the bacterial colonies that trigger the inflammatory cascade in the first place.
Flossing and Clot Prevention
Cleaning between the teeth daily is just as vital as brushing. The American Heart Association (AHA) and related research underscore the necessity of daily flossing or using interdental cleaners, suggesting it may specifically lower the risk of stroke caused by blood clots and irregular heartbeats (such as atrial fibrillation).
Flossing addresses the deep reservoirs of plaque located between teeth and under the gum line that brushing cannot reach.
These areas are prime locations for the development of periodontal disease, making daily flossing a direct, targeted action to remove the bacterial source linked to increased procoagulant risk. The benefit of regular flossing is recognized as an affordable, accessible, and healthy habit.
Pillar 3: Lifestyle Optimization
Systemic health, including vascular risk, is heavily influenced by lifestyle factors that directly impact the oral microbiome and immune response.
Diet and Caries Control

A healthy diet that minimizes the intake of sugary beverages and refined, starchy snacks is essential for mitigating the oral health stroke risk. Sugar serves as the primary fuel source for the bacteria that cause both dental caries and, subsequently, severe gum disease.
Reducing this intake limits the acid production that creates cavities and starves the overall bacterial load in the mouth, reinforcing the protective effects of proper hygiene.
Tobacco and Vascular Toxin Avoidance

Avoiding all forms of tobacco use is a non-negotiable step for comprehensive stroke prevention. Smoking, dipping, chewing tobacco, vaping, and hookah use all severely affect the health of the gums and drastically increase overall cardiovascular risk.
Tobacco constricts blood vessels, impairs immune function, and significantly accelerates the progression of periodontal disease, thereby compounding the inflammation that drives ischemic stroke.
Beyond Brushing: The Future of Stroke Prevention Requires Integrated Care
The Medical Community’s Paradigm Shift

The strength and consistency of the 2025 findings, particularly the 86% risk figure and the clear inflammatory pathway, necessitate a profound shift in how medical professionals approach vascular risk assessment.
Leading neurologists are now recommending “integrating dental care into medical risk assessments to reduce vascular risks”. This means dental health can no longer be seen as an isolated specialty. The connection between chronic infection and vascular inflammation is too strong to ignore.
For healthcare providers, this requires asking detailed questions about a patient’s dental status, including their frequency of dental visits, and potentially screening high-risk stroke patients for periodontal indicators, or even measuring inflammatory markers like CRP.
The goal is to view the mouth as a primary, easily modifiable port of entry for systemic inflammation. By controlling the bacterial load, clinicians are addressing a fundamental component of the processes that drive atherosclerosis and blood clotting, key factors in ischemic stroke etiology.
Addressing the Global Public Health Burden

The implications of prioritizing oral health are massive, particularly when considering the global burden of stroke. The estimated global cost of stroke exceeds US$890 billion, demonstrating the monumental economic weight of this condition.
The World Stroke Organization notes that behavioral risks, which include poor oral hygiene, constitute 35.0% of all strokes worldwide.
Improving oral hygiene is an accessible, affordable, and universally applicable preventative measure. The simple habits of brushing, flossing, and seeking regular dental check-ups—the habits that correlate with an 81% reduction in the combined risk factor—represent an incredibly cost-effective public health strategy when weighed against the costs of stroke treatment and rehabilitation.
Widespread public education and the implementation of this integrated health message are essential to close the gap between specialist knowledge (the 86% statistic) and general public awareness.
Patient Advocacy: Guiding Your Own Integrated Care

Individuals must become active participants in this integrated healthcare model. The first step involves recognizing that the oral health stroke risk is real, even if symptoms are absent. Since periodontal disease often progresses silently, assuming the risk and seeking proactive screening is the safest approach.
Patients are encouraged to initiate dialogue with both their dentist and their primary care physician. Informing a primary care provider about any diagnosis of gum disease or chronic cavities ensures that their vascular risk profile is complete.
Patients may also ask their physicians about their baseline systemic inflammation markers, such as CRP levels, and discuss whether improving dental health could be a therapeutic target to lower those levels.
While the original 2025 study noted the limitation of assessing oral health only once at the the evidence underscores that any action taken now to improve dental health offers a profound opportunity to modify future vascular outcomes and prevent the devastating consequences of cavities and brain damage.
Conclusion: Protect Your Brain, Starting with Your Teeth
The new data confirms that chronic oral infection, specifically the highly dangerous combination of periodontal disease and untreated cavities, acts as a systemic inflammatory engine that dramatically increases the likelihood of an ischemic stroke.
The 86% higher risk identified in 2025 is not a coincidence; it is the direct result of an inflammation pathway that fuels blood clots and arterial hardening.
The evidence points to a clear and immediate preventative strategy. The path to protection is simple and effective, starting with the immediate adoption of consistent home care and professional vigilance.
Do not wait for symptoms to manifest; schedule a dental check-up now to screen for gum disease and untreated cavities, eliminating the chronic source of infection.
Commit to the ADA’s two-minute brushing rule and daily flossing as a non-negotiable routine. Your oral health stroke risk is real, but it is entirely manageable, offering one of the most accessible and high-impact preventative health opportunities available today. Prioritizing your gum disease and cavity treatment is prioritizing your long-term brain health.








