Shocking Link Revealed: Why Bad Dentures Are the #1 Hidden Cause of Malnutrition in Seniors (And It’s Not What You Think)
A 2025 investigation reveals a silent epidemic: millions of seniors face malnutrition, not from a lack of food, but from poor-fitting dental prosthetics.
This report exposes an unspoken struggle—a hidden, cyclical link connecting dental pain, nutritional deficiency, and social isolation. This is not an inevitable part of aging. Based on the latest 2025 clinical data, we provide an actionable guide for seniors and their caregivers to break this cycle.
This report details how to identify the warning signs and outlines concrete solutions to fix the fit, the food, and the finances, empowering older adults to reclaim their health, their confidence, and their plate.
The Scale of a Silent Epidemic: The 2025 Data
The connection between oral health and systemic health is no longer a theory; it is a measurable crisis. For millions of older adults, the unspoken struggle with ill-fitting dentures is the primary driver of a decline into malnutrition, frailty, and social withdrawal.
A Crisis in Numbers: Dentures and Malnutrition in 2025

The problem is one of immense scale. By the end of 2025, an estimated 42.46 million Americans will use dentures. This is not a niche medical device; it is a daily reality for a significant portion of the population, particularly seniors. Current data indicates that 57% of all senior citizens wear dentures.
This population is sourced from a widespread underlying condition: edentulism, or complete tooth loss. Nearly one in four individuals over the age of 60 suffers from this condition.
Data from the Centers for Disease Control and Prevention (CDC) further specifies that 13.2% of all adults aged 65 and older have experienced complete tooth loss. These individuals are the primary candidates for the dentures that are, in many cases, failing to serve their core purpose.
The critical, and often missed, connection is the direct line to malnutrition. A 2024/2025 study identified that 23.5% of participants who wear dentures are at risk of malnutrition.
A separate, large-scale 2024/2025 study involving 3,876 older adults found that 33.6% of the entire cohort were malnourished. This same study demonstrated a significant statistical link between malnutrition and oral health problems, including broken teeth and, most notably, chewing difficulties.
The Real Culprit: Why “Bad” Dentures Are the Norm

The central problem is not the concept of dentures, but the prevalence of old, ill-fitting dentures. This reveals a profound misunderstanding of how dentures function.
Many patients and even some practitioners treat a new denture as a permanent, one-time “fix,” similar to an artificial hip. The reality is that the mouth is a dynamic environment.
When natural tooth roots are lost, the jawbone (alveolar ridge) is no longer stimulated, and it begins a process of resorption, or shrinkage. The gum tissue recedes with it. This means that a denture that fit perfectly in 2020 is almost guaranteed to be loose and ill-fitting by 2025.
This biological fact is met with a harsh economic reality. While dentists recommend replacing or relining dentures every five years, a staggeringly low 15% of the edentulous population gets new ones made each year.
The Hidden Handicap: More Than Just a Meal
The physical consequences of malnutrition are well-documented. However, the psychological and social trauma associated with ill-fitting dentures is often a more immediate and debilitating burden.
“A Hidden Disability”: The Emotional Tunnel of Tooth Loss

A landmark 2024 study from the University of Sheffield provides the critical language to understand this experience, labeling the struggle with dentures as a “hidden disability”. The researchers mapped the patient’s journey, identifying a phase they call “The Emotional Tunnel”.
This journey is not merely one of physical adaptation but of profound psychological distress. The study identified deep-seated feelings of “self-consciousness, shame, anger, or fear”.
Tooth loss itself is described as a “hugely traumatic” event. This “emotional weight” impacts self-esteem and, crucially, leads to “reduced social interactions” as individuals become afraid to eat, speak, or even smile in public.
The 2025-era understanding of this problem is shifting. Research now highlights the importance of “empathy from dentists”, the development of “new patient questionnaires” to screen for these psycho-social challenges, and the study of “psychological resilience” in denture patients.
This signals a necessary evolution in dental care: success is not just a mechanical fit, but a restoration of the patient’s confidence and social well-being.
Actionable Guide Part 1: The 10-Second Self-Check
The first step to solving the problem is identifying it. Many seniors have been told, or have come to believe, that pain and discomfort are a normal, unavoidable part of wearing dentures. This is false. Pain is a signal, not a sentence. Discomfort is a sign that the prosthetic is no longer matched to the mouth.
Is Your Denture Failing You? A 2025 Warning Sign Checklist
Denture Fit Warning Signs!
What It Really Means:
This is the #1 sign. Your gums and jawbone have shrunk, and the denture no longer matches your mouth’s shape. This is NOT a failure of your adhesive.
Your Action Step:
Call your dentist and ask for a “fit evaluation” or “reline consultation.”
What It Really Means:
This is a LATE-STAGE sign. Your denture is rubbing unevenly and creating wounds. Ignoring this can lead to serious infections.
Your Action Step:
See your dentist immediately. This is an urgent problem. Do not “tough it out.”
What It Really Means:
You lack stability. This is a direct link to nutritional deficiency and muscle loss (sarcopenia).
Your Action Step:
See your dentist. In the meantime, start a soft, nutrient-dense food plan.
What It Really Means:
Food particles and bacteria are trapped under the loose-fitting denture. This is a primary cause of fungal infections (Denture Stomatitis).
Your Action Step:
See your dentist. Your denture needs a professional cleaning, and you need to be screened for infection.
What It Really Means:
The denture is so loose it’s interfering with your tongue and lip movement. This is a clear sign of a severe fit issue.
Your Action Step:
See your dentist. This is a quality-of-life issue that can lead to social isolation.
What It Really Means:
A “sunken” or “collapsed” look signals advanced bone loss. The denture is not providing adequate support for your lips and cheeks.
Your Action Step:
See your dentist. This is a sign you need to discuss all options (relines, new dentures, implants).
What It Really Means:
You are using adhesive as a crutch for a structural failure. Adhesives are meant to enhance the seal of *well-fitting* dentures, not fill gaps.
Your Action Step:
This is a temporary fix for a permanent problem. Schedule a reline appointment.
This checklist, based on 2025 dental guidance, can help a user or caregiver identify a poor fit. The most obvious sign of a problem is not necessarily pain, but slippage. Pain is a late-stage indicator that develops after the slipping and rubbing have caused a wound. Recognizing the early warning signs is critical.
Actionable Guide Part 2: Reclaiming Nutrition Today
A dental appointment may be weeks away. For a senior suffering from a poor fit today, nutritional intervention cannot wait. This section provides an immediate “damage control” plan.
The Foods You’re Avoiding (and the Nutrients You’re Missing)

When chewing is painful or difficult, the first foods to be eliminated from the diet are those that are hard, crunchy, or fibrous. This is a nutritional catastrophe. The “hard-to-chew” list is a “who’s who” of essential nutrition:
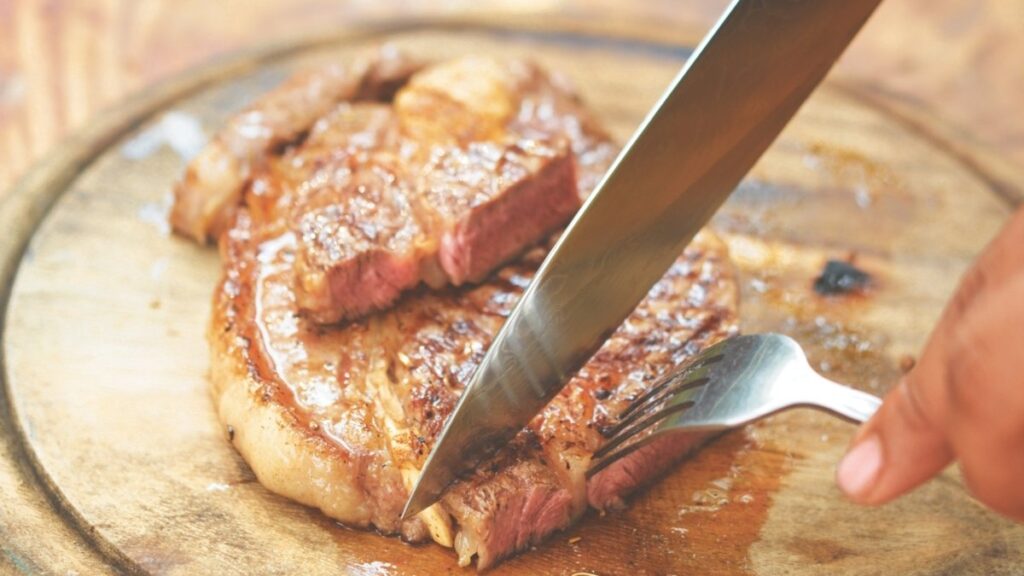
- Steak and other meats (protein, iron, B12)
- Chicken (especially with bones) (protein)
- Nuts and seeds (protein, healthy fats, magnesium)
- Raw fruits and crunchy vegetables (fiber, vitamins A and C)
- Hard cheeses (calcium)
The consequence of avoiding these foods is a predictable and dangerous profile of nutritional deficiencies. 2025 research confirms that individuals with chewing problems are most commonly deficient in: Protein, Calcium, Iron, Vitamin A, Riboflavin, and Magnesium.
The link is not anecdotal; it is statistically proven. Recent longitudinal studies show that self-reported difficulty in chewing hard food significantly increases the odds of being at risk for malnutrition (Odds Ratio = 1.64) and severe weight loss (Odds Ratio = 1.72).
The 2025 High-Protein, Soft-Food Solution
Many seniors and caregivers fall into the “soft food trap.” They rightly identify the need for soft foods but default to items that are high in carbohydrates and sugar but nutritionally barren. A diet of mashed potatoes, ice cream, pudding, and white bread will provide calories but will accelerate malnutrition and muscle loss.
The 2025 strategy is not about soft food; it is about nutrient-dense, high-protein soft food. The goal is to replace the nutrients being missed from the hard-to-chew foods.
5 High-Protein, Easy-Chew Recipes for 2025
The Nutrient-Dense Soft Food Solution
The Problem: The “Soft Food Trap” (pudding, ice cream, white bread) provides calories but accelerates muscle loss.
Your 2025 Easy-Chew Swaps:
- Moist Meatloaf
- Ground Meats in gravy
- Pureed Lentil Soup
- Pureed Bean Soup
- Soft Scrambled Eggs
- Blended Chicken/Turkey
Your 2025 Easy-Chew Swaps:
- Greek Yogurt (smooth)
- Cottage Cheese
- Silken Tofu (in smoothies)
- Protein-Enriched Oatmeal
- Protein Shakes
Your 2025 Easy-Chew Swaps:
- Mashed Sweet Potatoes
- Mashed Avocado
- Applesauce (unsweetened)
- Steamed/Mashed Carrots
- Butternut Squash Soup
- Cream of Broccoli Soup
These simple recipes, drawn from geriatric nutrition guides, are packed with protein and easy to consume.
Veggie-Packed Scrambled Eggs: Add finely chopped, cooked vegetables such as spinach, zucchini, or bell peppers to scrambled eggs for a colorful, nutrient-dense breakfast.
Pureed Lentil Soup: Simmer red lentils with garlic, onions, and spices, then blend until smooth for a hearty, protein-rich soup.
Herb Cottage Cheese Spread: Mix cottage cheese with fresh dill, parsley, or chives. Spread it on soft bread or use it as a dip for soft-cooked (steamed) vegetables.
High-Protein “Power Oatmeal”: Elevate standard oatmeal by mixing in a scoop of unflavored protein powder, a tablespoon of smooth nut butter (seed paste), or chia seeds.
Moist & Tender Meatloaf: Prepare meatloaf with ground hamburger, turkey, or beef, using plenty of moisture (e.g., broth, gravy, soaked breadcrumbs) to ensure a soft, non-chewy texture.
A critical, non-obvious tool in this fight is the right equipment. A simple, affordable hand blender, food processor, or slow cooker can be the most important investment for a senior’s nutritional health.
These tools empower them to take healthy foods—like a chicken breast or a pot of vegetables—and transform them into a chewable, digestible, and nutrient-rich meal, preserving both dignity and variety.
Actionable Guide Part 3: Fixing the Fit for Good
Nutritional strategies are vital “damage control” but do not solve the underlying mechanical problem. A three-tiered approach exists for fixing the fit, ranging from temporary patches to permanent solutions.
Temporary Fixes: Best Adhesives for 2025 (And What They Can’t Do)

Adhesives are a “crutch,” not a solution. 2025 product reviews emphasize that adhesives are intended to enhance the seal of well-fitting dentures, not to fill the gaps in ill-fitting ones. If a user must reapply adhesive multiple times a day or is still experiencing slippage, the denture does not fit.
For temporary security while awaiting a dental appointment, 2025 reviews suggest:
Best Overall Cream: Poligrip Ultra. It is zinc-free, provides a strong hold, and has an easy-to-use nozzle.
Best Powder: Fixodent Extra Hold. Powders are often preferred for a less “gooey” feel and easy application.
Best for Sore Gums: Y-Kelin Denture Adhesive Cushion or Sea-Bond Secure Adhesive Seals. These products provide a soft cushion. However, the need for this type of product is a definitive sign of a severe fit problem that requires immediate dental attention.
The Short-Term Fix: What is a Denture Reline (and 2025 Costs)

For most seniors with loose conventional dentures, the correct solution is a reline. This is a standard, routine maintenance procedure.
A reline does not replace the denture; it resurfaces the inside of the denture base with new material to make it conform perfectly to the new, shrunken shape of the user’s gums. This procedure is typically required every one to two years.
Soft Reline: Uses a pliable, cushioned material for those with tender or sore gums. 2025 costs typically range from $250 to $500.
Hard Reline: Uses a durable acrylic material similar to the denture base itself. This is more long-lasting, with 2025 costs ranging from $300 to $900.
The Long-Term Solution: Are Implant-Supported Dentures Worth It?

The “gold standard” 2025 solution that permanently addresses the root causes of instability and bone loss is the implant-supported denture. New technologies like 3D printing, AI-driven smile design, and advanced biocompatible materials are making these options more precise and accessible.
This solution involves placing two or more dental implants into the jawbone, which then serve as “snaps” or “anchors” for the denture.
A definitive 2025 NIH-published study provides a clear “YES” to their value, comparing patient satisfaction between implant-supported and conventional dentures:
Stability: Implant users reported a 9.2/10 satisfaction, versus 5.8/10 for conventional users.
Comfort: Implant users reported an 8.9/10 satisfaction, versus 6.5/10 for conventional users.
Chewing Hard Food: This is the most critical finding for nutrition. Implant users reported an 8.4/10 ability, versus a 5.9/10 for conventional users.
This data proves that implant-supported dentures solve the core nutritional problem by restoring chewing function.
Costs are highly variable. A “snap-in” overdenture (removable) may range from $5,000 to $20,000. A “fixed” or “All-on-4” prosthesis (permanent) can range from $20,000 to $50,000 or more per arch.
This data allows for a clear, cost-benefit analysis for any senior or caregiver weighing their options.
Overcoming the Barriers: Your 2025 Action Plan
Knowing the solutions is only half the battle. Accessing them requires a clear plan for navigating the healthcare and financial systems.
The 2025 “Dual-Track” Solution: Dentist + Dietitian

A dentist fixes the mechanical problem. A Registered Dietitian Nutritionist (RDN) fixes the nutritional problem. Both are required.
A 2025 consensus statement from the Academy of Nutrition and Dietetics demands “evidence-based individualized nutrition care” and “expanded reimbursement” for these exact services. A patient or caregiver should ask their primary care physician for a referral to an RDN to develop a personalized eating plan.
The 2025 solution for this is Telehealth. For seniors with mobility or transportation challenges, this is a revolutionary change.
A 2025 guide from telehealth.hhs.gov promotes the use of virtual care for geriatric nutrition, including “virtual assessments of weight, muscle loss, and chronic conditions”. This expert help can be accessed from the comfort of home.
You Are Not Alone: Financial Aid and Support Resources
Financial Aid For the millions of seniors who cannot afford a $400 reline, let alone implants, a patchwork of public and private aid exists.
Dental Lifeline Network (DLN): This is the single most important resource. DLN is a national non-profit organization of volunteer dentists that provides free, comprehensive dental care (including dentures) for seniors aged 65+, the disabled, or the medically fragile.
How to Apply to DLN (The 2025 Reality): The application process requires persistence. An applicant must go to the DLN website, check if their state and county are currently “open” and accepting applications, and then complete a detailed online or paper application.
The waitlist is long—often months to a year or more. This is a process that a caregiver or family member should “project manage” for the senior.
State & Local Aid: Many states have their own dedicated funds. Examples include the Colorado Dental Health Care Program for Low-Income Seniors and community programs in states like Michigan. The most effective action is to search online for ” senior dental program” or ” low-income dental care.”
Community Health Centers: Federally-funded community health centers provide dental services on a sliding-scale (ability-to-pay) basis.
Peer Support To combat the “hidden disability” and “shame” of tooth loss, connection is vital. Online blogs and private peer-support forums (such as private Facebook groups) provide a safe, anonymous space.
These communities allow new and existing denture wearers to ask sensitive questions, share experiences, and find encouragement from people who understand the struggle.
A Final Word: Do Not Accept Pain as Normal
The evidence is clear. The connection between a sore mouth and a weak, malnourished body is not a personal failure; it is a predictable medical outcome. Pain is a signal, not a sentence. Discomfort is a warning sign of a correctable problem.
This issue is not one of vanity. It is a serious, systemic health crisis that robs millions of seniors of their health, dignity, and joy. Using the resources in this report—the self-check list, the nutrient-dense food swaps, and the financial aid list—is the first step toward reclaiming health.
The final, urgent call to action is to make two phone calls: one to a dentist to schedule a fit evaluation, and one to a loved one or caregiver to share this article and ask for their support.








