9 out of 10 Seniors Get This Wrong: The Shocking Truth About Why They Fail at Eating Well (And How You Can Win)
Malnutrition in older adults is a silent and pervasive crisis, often mistaken for an inevitable consequence of aging. It is far more than the simple sensation of hunger; it is a complex medical and social condition that quietly undermines health, erodes independence, and diminishes quality of life.
Proper nutrition is not a luxury but the very bedrock of vitality, strength, and the ability to live independently in one’s later years. When an older person struggles with nutrition, it is rarely a personal failing or a simple loss of appetite.
Instead, it is typically the result of a confluence of physiological changes, hidden medical conditions, and challenging life circumstances.
This report serves as a comprehensive guide to demystify the multifaceted causes of senior malnutrition and to provide a clear, actionable roadmap to effective, life-sustaining solutions.
By understanding the intricate web of factors at play, older adults, their families, and caregivers can become empowered advocates for better health, moving beyond the empty plate toward a future of strength and well-being.
The Body's Changing Needs: A New Nutritional Blueprint

As the body ages, its fundamental relationship with food and nutrients undergoes a significant transformation. These changes create a unique nutritional paradox: while older adults generally require fewer calories, their need for specific, high-quality nutrients actually increases. This shift is driven by several key physiological developments.
First, the body's metabolism naturally slows with age, and a more sedentary lifestyle often leads to a decrease in overall energy requirements.
This means that consuming the same number of calories as in one's younger years can lead to weight gain, particularly an increase in adipose tissue around the body's central area. However, this reduced need for total energy masks a more critical change.
When the Body Fights Itself: Hidden Saboteurs of Senior Health
Often, the root causes of malnutrition are not simply dietary choices but specific, diagnosable medical conditions that actively sabotage the body's ability to use the food it consumes.
Symptoms frequently dismissed as "just getting older"—such as weakness, fatigue, or confusion—can be warning signs of underlying pathologies that require medical intervention. Two of the most significant and often overlooked of these conditions are sarcopenia and atrophic gastritis.
1. Sarcopenia: The Silent Loss of Strength
Sarcopenia is not merely the weakness that comes with age; it is a progressive musculoskeletal disease defined by a significant loss of muscle mass, strength, and physical performance.
This condition directly threatens an individual's ability to perform the basic activities of daily living, transforming simple tasks into monumental challenges. The signs are often subtle at first but become increasingly debilitating.
The consequences of untreated sarcopenia are severe. The progressive loss of strength and balance is strongly associated with a greater incidence of falls, which can lead to fractures, hospitalizations, and a subsequent loss of independence. It is a primary driver of frailty and a key risk factor for needing long-term care.
2. Atrophic Gastritis: The Gut's Absorption Barrier
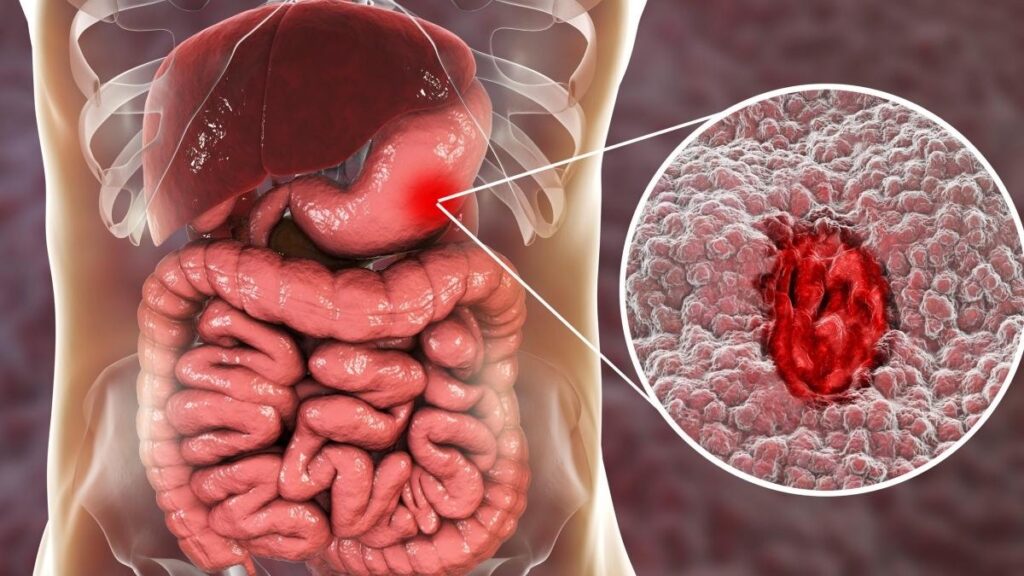
While sarcopenia affects the body's ability to use nutrients to build strength, another hidden condition, autoimmune metaplastic atrophic gastritis (AMAG), prevents those nutrients from being absorbed in the first place.
AMAG is an inherited autoimmune disease in which the body's immune system mistakenly attacks the lining of the stomach, specifically the parietal cells.
First, the loss of parietal cells leads to hypochlorhydria, a dramatic reduction in the production of stomach acid. Stomach acid is essential for breaking down food and releasing nutrients, particularly Vitamin B12, from the proteins they are bound to.
Second, parietal cells are responsible for producing a protein called "intrinsic factor," which is indispensable for the absorption of Vitamin B12 in the small intestine.
The resulting Vitamin B12 deficiency can develop slowly and insidiously, producing a wide spectrum of symptoms that are often misattributed to other causes. The effects can be devastating and manifest in several ways:
Physical Symptoms: Pervasive fatigue, weakness, unexplained weight loss, a smooth or sore tongue, changes in taste, loss of appetite, and various gastrointestinal complaints like nausea or flatulence.
Neurological Symptoms: These often occur independently of anemia and can include paresthesia (numbness or tingling in the hands and feet), gait abnormalities, balance problems, and muscle weakness.
Cognitive and Psychological Symptoms: The neurological impact can be severe, leading to altered mental status, cognitive defects, depression, irritability, paranoia, and even delusions—a collection of symptoms sometimes referred to as "megaloblastic madness".
Because there are no specific early symptoms that point directly to atrophic gastritis, it is often discovered incidentally during an endoscopy performed to investigate unexplained anemia or abdominal discomfort.
A definitive diagnosis is made through a biopsy of the stomach lining, often supplemented by blood tests that check for the presence of antibodies against parietal cells and intrinsic factor.
The Web of Causes: Beyond the Kitchen Table
Malnutrition in older adults is rarely a purely medical issue. It is deeply embedded in the social, economic, and environmental context of a person's life.
The internal, physiological challenges of aging are often compounded by external factors that create powerful barriers to good nutrition. Understanding this broader web of causes is essential to developing holistic and effective solutions.
The High Cost of Being Alone: Social Isolation vs. Loneliness

While often used interchangeably, social isolation and loneliness are distinct concepts with profound and separate impacts on health. Clarifying this distinction is crucial to understanding their role in senior malnutrition.
Social Isolation is the objective, physical state of having few social relationships or infrequent contact with others. It is a measurable lack of connection that can arise from mobility challenges, hearing loss, or the loss of friends and family members.
Loneliness is the subjective, distressing feeling of being alone or disconnected from others. It reflects the gap between a person's desired level of social connection and their actual level. An individual can feel lonely even when surrounded by people if they lack deep, meaningful relationships.
This is a widespread problem, with data showing that about one in three adults in the U.S. reports feeling lonely. Both conditions pose a serious threat to mental and physical health.
Research has linked social isolation and loneliness to an increased risk for a host of serious conditions, including heart disease, stroke, type 2 diabetes, depression, anxiety, dementia, and even premature death.
Navigating Food Insecurity: When Healthy Food is Out of Reach

For many seniors, the challenge is not a lack of desire to eat well, but a lack of access. Food insecurity in this population is not simply about having no food; it is a complex problem rooted in a combination of physical, financial, and logistical barriers.
Several factors contribute to this growing issue. Chronic health conditions can make the physical acts of shopping for groceries or standing in a kitchen to cook feel overwhelming. Limited or nonexistent transportation options can turn a simple trip to the supermarket into a significant logistical hurdle, particularly for those living in rural areas.
The health consequences of this insecurity are stark and well-documented. Food-insecure seniors are 50% more likely to have diabetes, 60% more likely to have congestive heart failure or a heart attack, and three times more likely to suffer from depression.
This creates a vicious cycle where poor health contributes to food insecurity, and the resulting poor nutrition further exacerbates chronic health conditions.
A Toolkit for Thriving: Finding the Right Nutritional Support

Understanding the complex causes of senior malnutrition is the first step; the next is to connect individuals with the right resources. A robust network of community, government, and commercial programs exists to provide nutritional support. These programs are not one-size-fits-all.
They represent a spectrum of services designed to meet different needs, from financial assistance for groceries to medically tailored prepared meals. Navigating these options can empower older adults and their caregivers to build a resilient foundation for better health.
Community and Government-Funded Programs: Your First Line of Support
For many older adults, publicly funded programs are the most accessible and affordable starting point for nutritional assistance. These services are designed to address the core issues of food access, affordability, and social isolation.
1. Meals on Wheels: More Than a Meal

What it is: Meals on Wheels is a nationwide network of community-based programs that deliver prepared meals to individuals at home who are unable to purchase or prepare their own food.
Crucially, the program serves a dual mission: it provides essential nutrition while also offering a friendly visit and a vital safety check, directly combating the health risks of social isolation.
Eligibility: The primary recipients are adults aged 60 and over who have mobility challenges that make it difficult to shop, cook, or socialize. Eligibility is generally determined by an individual's need for nutritional support, not strictly by their financial status, though criteria can vary by local provider.
Services and Cost: The core service is home-delivered meals, but many local programs also offer community dining at senior centers, nutrition counseling, transportation assistance, and even pet food delivery.
Depending on the local program and an individual's circumstances, meals may be free, offered for a suggested donation, or paid for on a sliding scale based on income.
The Challenge: The demand for these services far outstrips available resources. Meals on Wheels programs across the country are facing a funding crisis, with approximately one in three providers reporting a waitlist for meals.
In some areas, seniors may have to wait up to eight months to receive services, a critical delay that highlights the urgent need for increased public and private support.
2. SNAP (Supplemental Nutrition Assistance Program): Empowering Grocery Choices

What it is: SNAP is a federal program that provides monthly funds on an Electronic Benefit Transfer (EBT) card, which functions like a debit card, to be used for purchasing groceries at authorized stores. The program empowers recipients with the autonomy and dignity of choosing their own food.
Eligibility (for Oct. 2025 - Sept. 2026): Eligibility is based on household size, income, and countable resources. However, special rules make it easier for seniors (defined as age 60 or older) and individuals with disabilities to qualify. The household resource limit is higher—$4,500 in a bank account, compared to $3,000 for other households.
Income Limits: For the period of October 1, 2025, through September 30, 2026, a one-person household must have a gross monthly income at or below $1,696 to be eligible.
How to Apply: Individuals must apply in the state where they live. The application can typically be completed online through the state agency's website, at a local office, or over the phone. The process requires an eligibility interview and verification of the information provided.
3. CSFP (Commodity Supplemental Food Program): Monthly Nutrition Delivered

What it is: CSFP is a federal program administered by states that works to improve the health of low-income seniors by supplementing their diets with a monthly package of nutritious foods from the U.S. Department of Agriculture (USDA). In some states, the program is known by other names, such as "Everyday Eats" in Colorado.
Contents: The monthly food package is designed to provide nutrients often lacking in the diets of older adults, such as vitamins A and C, calcium, and iron. A typical box contains a variety of shelf-stable items, including cereal, oats, pasta, rice, cheese, peanut butter, canned meats or fish, canned fruits and vegetables, and milk.
Eligibility: The program is specifically for low-income individuals who are at least 60 years of age. Income eligibility guidelines are set by the state but are typically at or below 130% of the Federal Poverty Level, though some states may extend this to 150%.
How to Apply: CSFP is not available in all counties. Interested individuals must apply through local agencies, such as food banks or community action organizations, that partner with the state to distribute the food packages.
4. SFMNP (Senior Farmers' Market Nutrition Program): Accessing Fresh, Local Foods

What it is: SFMNP is a seasonal program, typically running in the summer months, that provides low-income seniors with coupons, vouchers, or e-benefit cards to purchase fresh, locally grown produce.
Eligible foods include fruits, vegetables, fresh-cut herbs, and raw honey, available at participating farmers' markets, roadside stands, and community-supported agriculture programs.
Dual Benefit: The program serves two important functions: it improves the nutritional intake of older adults by giving them access to fresh foods, and it simultaneously supports local farmers and agricultural economies.
Eligibility: To participate, an individual must typically be 60 years of age or older and have a household income at or below 185% of the Federal Poverty Level. The program is not available in all counties, and funding is limited, so vouchers are not guaranteed even for those who meet the criteria.
How to Apply: The application window is usually in the spring and can close quickly due to high demand. Interested seniors should contact their local Area Agency on Aging early in the year to find out if the program is available in their area and how to apply.
The Growing World of Meal Delivery: A Comparative Guide
Your Meal Delivery Guide!
Mom's Meals
Focus: Medically tailored meals for chronic conditions
Click to Open!
About Mom's Meals
A leader in "Food as Medicine," offering refrigerated meals by dietitians for renal, diabetic, heart, and cancer support. Customers can choose from over 50 options.
- High degree of medical specificity
- Good food quality & customer service
- A la carte (no subscription)
- Heavy boxes
- Difficult packaging for dexterity issues
Magic Kitchen
Focus: Diet-specific frozen meals for seniors & medical needs
Click to Open!
About Magic Kitchen
Specializes in frozen meals for complex medical needs, including renal and dialysis-friendly diets. Offers both complete meals and a la carte items with no subscription.
- Wide variety & generous portions
- Caters to complex renal/dialysis needs
- Flexible ordering (no subscription)
- High shipping costs (starts ~$20)
- Low-sodium options can be bland
Silver Cuisine
Focus: Doctor-designed frozen meals for adults 50+
Click to Open!
About Silver Cuisine (by BistroMD)
The senior brand of BistroMD, offering 150+ doctor-designed frozen meals for heart health, diabetes, etc. Partners with AARP for discounts.
- Doctor-designed menus
- AARP discounts available
- Free shipping on orders over $99
- High shipping cost ($19.95) under $99
- Portions can be small
Factor
Focus: Fresh, convenient meals for active lifestyles
Click to Open!
About Factor
Best for active, health-conscious people who want fresh (never-frozen), ready-to-eat meals. Operates on a weekly subscription with plans like Keto and High-Protein.
- Fresh (not frozen) & flavorful
- Easy-to-manage subscription
- Good for active lifestyles
- Less focus on senior medical diets
- Portions can be small
- Menu template can feel repetitive
How to Choose the Right Service
The key is to match an individual's specific circumstances. A person with advanced kidney disease needs a specialized service like Mom's Meals or Magic Kitchen. An active adult who just finds cooking burdensome might prefer the fresh, convenient meals from Factor. Always match the financial, medical, and logistical needs to the service.
For those who may not qualify for government assistance, have highly specific medical dietary needs, or simply seek greater convenience, commercial meal delivery services have emerged as a powerful solution.
In-Depth Service Reviews

Mom's Meals: Operating under the principle of "Food as Medicine," Mom's Meals is a leader in providing medically tailored, refrigerated meals designed by registered dietitians to support the management of chronic conditions.
Customers can choose from a wide menu of over 50 options, including renal-friendly, diabetic-friendly, heart-friendly, and cancer support meals.
Magic Kitchen: This service specializes in frozen meals catering to a broad array of dietary needs, with a particular strength in providing options for those with complex medical requirements, such as renal diets and dialysis-friendly meals.
It offers both complete meals and a la carte items, allowing for flexibility in ordering without a subscription.
Silver Cuisine (by BistroMD): As the senior-focused brand of the well-regarded BistroMD service, Silver Cuisine offers a rotating menu of over 150 doctor-designed, chef-prepared frozen meals tailored to the nutritional needs of adults over 50. It provides plans for heart health, diabetes, and menopause, among others.
Factor: Factor is best positioned for active, health-conscious seniors who prioritize convenience and fresh, flavorful food over highly specific medical diet management.
The service operates on a weekly subscription model and delivers fresh, never-frozen meals that are ready to heat and eat. Its menu focuses on plans like Keto, High-Protein, and Carb-Conscious.
Building a Foundation for a Healthier Future

Senior malnutrition is a formidable challenge, but it is not an insurmountable one. The solution lies in a holistic approach that recognizes its complex medical, social, and economic roots.
It requires moving beyond the misconception that weakness and confusion are normal parts of aging and instead treating them as potential signs of underlying, addressable conditions.
By being proactive, informed, and willing to seek help, older adults and their caregivers can build a strong foundation for health, independence, and a higher quality of life. The following checklist provides a clear, actionable path forward.
Action Checklist for Seniors and Caregivers:

Recognize the Warning Signs: Be vigilant for the key symptoms of sarcopenia (e.g., progressive weakness, difficulty rising from a chair, a weak grip) and Vitamin B12 deficiency (e.g., persistent fatigue, confusion, memory problems, numbness or tingling in the extremities). Do not dismiss these changes as inevitable consequences of aging.
Talk to a Doctor: Proactively discuss these symptoms with a healthcare provider. Specifically ask for a screening for sarcopenia and a blood test to check Vitamin B12 levels. This is especially important if there is a history of gastrointestinal issues, as this can point toward conditions like atrophic gastritis.
Assess Social Connection: Take an honest look at the level of social interaction in daily life. Evaluate both the quantity of contact (social isolation) and the quality of relationships (loneliness).
If a deficit exists, explore resources like local senior centers, volunteer opportunities, or community meal sites, which provide both nutrition and social engagement.
Review the Budget and Barriers: Identify the primary obstacles to consistent, good nutrition. Is the main issue the cost of healthy food? Is it a lack of transportation to the grocery store? Or is it the physical difficulty of preparing meals? Pinpointing the specific barrier is the first step to finding the right solution.
Explore the Toolkit: Use the detailed information in Part III of this report to identify the one or two most relevant support programs to investigate first.
Start with the government-funded options like SNAP, CSFP, or Meals on Wheels if income or mobility are primary concerns. If highly specific medical diets are required, explore the specialized commercial services.
Advocate: For those in a position to do so, become an advocate. Given the long and growing waitlists for vital services like Meals on Wheels, contacting local and national congressional representatives to urge for increased funding can make a significant difference for thousands of vulnerable seniors in the community.
Conclusion: Claiming Your Victory for a Healthier, More Vibrant Life
The path to good nutrition in later life is undeniably fraught with challenges. The evidence is clear: a confluence of profound biological shifts, the quiet erosion of social connections, and a host of practical daily hurdles conspire to make eating well a formidable task.
Malnutrition and food insecurity are not minor concerns but widespread crises that threaten the health, independence, and vitality of millions of older adults. Yet, these challenges, however significant, are not insurmountable.
This report has illuminated the battlefield and provided a comprehensive playbook for victory. The core message is one of empowerment through knowledge and strategy.
The solution lies not in a single magic bullet, but in a multi-faceted approach: adopting a nutrient-dense eating pattern tailored to the body's changing needs; designing a personal food system that makes cooking for one efficient and sustainable; and strategically calling in reinforcements from the vast network of community and technological support systems available.








