Never Too Late: How Seniors Are Reversing Type 2 Diabetes Through Simple Diet Changes (Real Stories)
At 62, Martha was told her diabetes would only get worse. Two years later, she’s off all medications with normal blood sugar levels. She’s not alone—and age wasn’t the barrier doctors once thought it was.
If you’ve been told reversing type 2 diabetes is only for younger people, or fear it’s too late for meaningful change, think again. Research shows lifestyle interventions work even better for seniors, with those over 60 achieving a remarkable 71% risk reduction compared to 58% in younger adults.
This guide reveals evidence-based approaches specifically validated for older adults, real success stories from people like you, and safe strategies for achieving diabetes remission without juggling multiple medications.
Can You Really Reverse Diabetes After 60? Here’s What Science Says
Martha sat in her doctor’s office, staring at her blood sugar numbers. At 67, she’d just been diagnosed with type 2 diabetes. “I thought it was too late for me,” she remembers.

She was wrong.
Here’s what most doctors won’t tell you up front: people over 60 actually show better diabetes reversal results than younger adults. The CDC’s Diabetes Prevention Program found that seniors reduced their risk by 71% – better than any other age group.
Right now, 22-33% of adults over 65 have diabetes. But here’s the good news. Many are putting their diabetes into remission using simple diet changes and movement. No magic pills. No miracle cures. Just proven strategies backed by solid science.
This article will show you exactly how they did it.
What Does “Reversing” Diabetes Actually Mean?
Can You “Reverse” Diabetes?
Let’s clear something up right away. “Reversal” isn’t the same as “cured forever.”
When doctors talk about diabetes remission, they mean your blood sugar stays normal for at least 3 months without medication. Your body is working better. You feel better. But you still need to maintain the changes that got you there.
Think of it like this: if you break your leg and it heals, the bone is strong again. But if you jump off a roof, you’ll break it again. Diabetes works the same way.
Type 2 diabetes gets worse over time if you don’t do something about it. But here’s the key: the earlier you catch it, the better your chances. Your body can bounce back. Those little insulin-making cells in your pancreas? They’re not dead. They’re just tired and covered in fat.
Special Considerations for Older Adults

Your doctor might set different blood sugar targets for you than for younger people. This isn’t because they think you can’t do better. It’s because sudden drops in blood sugar can be dangerous, especially if you’re on certain medications.
Seniors also need to think about other health conditions. If you have heart disease, kidney problems, or take multiple medications, your approach needs to be more careful. But “more careful” doesn’t mean “impossible.”
Why Your Body Can Heal Itself (Even Now)
Your pancreas has these cells called beta cells. They make insulin. When you eat, these cells release insulin to handle the sugar in your blood.
But when fat builds up in your liver and pancreas, these cells can’t work right. They’re like workers trying to do their job in a cluttered room. Clear out the clutter, and suddenly they can work again.
In one study, people saw their diabetes reverse in just 7 days on a very low-calorie diet. Their beta cells started working again that fast. Another trial called DiRECT found that 46% of people achieved remission at 12 months. The people who lost 15kg or more? 86% of them reversed their diabetes.
Here’s something brand new from 2025: researchers found that people with prediabetes could achieve remission without even losing weight. How? By changing where their body stores fat. Moving fat away from organs lets those organs work better.
5 Eating Strategies That Work for Seniors
You’ve probably heard a dozen different diet plans. Let’s cut through the noise. Here are the approaches that actually have science behind them.
Very Low-Calorie Diets: Fast Results, Big Commitment

This means eating 625-850 calories daily for 2-5 months. Sound extreme? It is. But it works fast.
You MUST have doctor supervision for this. As your blood sugar improves, your medications need to change. Otherwise, your blood sugar can drop too low and make you dizzy, confused, or worse.
This approach isn’t right for everyone. If you’re thin already, have kidney disease, or take insulin, this might not be safe for you.
Mediterranean Diet: The Sustainable Choice

Remember PREDIMED? It’s a huge study that found the Mediterranean diet cut diabetes risk by 52%. People ate more fish, olive oil, nuts, vegetables, and whole grains. Less red meat and processed food.
The best part? A low-carb version of the Mediterranean diet works especially well if you were just diagnosed. And it’s way easier to stick with long-term than extreme calorie restriction.
Think of it as eating like people in Greece or Italy. Real food. Good fats. Plenty of plants. You can actually enjoy your meals.
Intermittent Fasting: Timing Matters

This isn’t about what you eat. It’s about when you eat.
The most studied approach for older adults is 16:8. You eat during an 8-hour window and fast for 16 hours. For example, eat between noon and 8 PM. Then fast until noon the next day.
Some people prefer alternate-day fasting or 24-hour fasts three times a week. Studies show this can lead to 10-18% body weight loss.
Critical warning: If you take diabetes medications, especially insulin, fasting can be dangerous. Your blood sugar can drop too low during fasting hours. Talk to your doctor first. They’ll need to adjust your medications.
Start slow. Try 12:12 first. Eat during a 12-hour window, fast for 12. Once that feels easy, move to 14:10, then 16:8.
Plant-Based Whole Food Diet: Less Weight Loss Needed

Here’s something interesting. People eating a whole food, plant-based diet need to lose less weight to see the same results as people on other diets.
Why? Plants are packed with fiber. They reduce inflammation. They help your gut bacteria. All of this improves how your body handles insulin.
You don’t have to go fully vegan. Just eat more vegetables, fruits, beans, and whole grains. Less meat and dairy. Skip the processed junk.
Simple Portion Control: The Easiest Start
Not ready for big changes? Start here.
Losing just 5-7% of your body weight significantly reduces diabetes risk. If you weigh 200 pounds, that’s only 10-14 pounds.
Eat 500-750 fewer calories each day. Add some walking. That’s it. No special foods. No restricted eating windows. Just smaller portions of what you already eat.
Move Your Body: It’s Not Optional

Diet gets 80% of the attention. But exercise is the secret weapon most people ignore.
You need 150 minutes of moderate activity each week. That’s 30 minutes, 5 days a week. Add strength training twice a week.
One study found something amazing. People who walked 10,000 steps daily and cut calories? More than half reversed their diabetes. The walking alone – without reaching their weight loss goal – still improved their blood sugar.
What Counts as Moderate Activity?
Move Your Body: Your Secret Weapon!
If you can talk but not sing while doing it, that’s moderate. Walking at a decent pace. Water aerobics. Dancing. Gardening if you’re really working.
Can’t do 30 minutes straight? Break it up. Three 10-minute walks work just as well. Your blood sugar doesn’t care if it’s all at once or spread out.
Start Where You Are

Maybe you haven’t exercised in years. That’s okay. Start with 5 minutes. Walk to the mailbox and back. Do chair exercises during commercials.
Add a little more each week. Your body will adapt. The goal isn’t to become an athlete. It’s to move more than you did yesterday.
Balance exercises matter too. They prevent falls. Strength training keeps your muscles strong so you can keep doing what you love.
Real People, Real Results

John Clary weighed 424 pounds at age 60. His doctor put him on medications for diabetes, acid reflux, high blood pressure, and high cholesterol.
He tried a low-carb diet with intermittent fasting. Lost 160 pounds. Got off every single medication. His doctor calls him “a modern-day miracle.”
Val Roulic lost 60 pounds after her diagnosis. Her blood sugar returned to normal. She also got off blood pressure medication. She joined the CDC’s Diabetes Prevention Program and stuck with it.
A woman in her 60s came to Dr. Feinsinger’s office with a fasting glucose of 333. That’s dangerously high. She was on insulin. Her doctor started her on a plant-based whole food diet and told her to walk every day.
Within months, her fasting glucose dropped to 87. That’s normal. She completely stopped taking insulin.
Mary Gronholz was 56 when her doctor warned her: “I see obese 60-year-olds in my practice. I don’t see obese 80-year-olds.” That woke her up.
She combined time-restricted eating with low-carb foods. Lost significant weight. Reversed both her diabetes and high blood pressure.
What These Stories Have in Common
None of these people did anything crazy. They picked one approach and stuck with it. They worked with their doctors. They made changes gradually. And they didn’t quit when progress felt slow.
They’re not special. They’re not superhuman. They just decided that feeling better was worth some effort.
Before You Start: Safety First
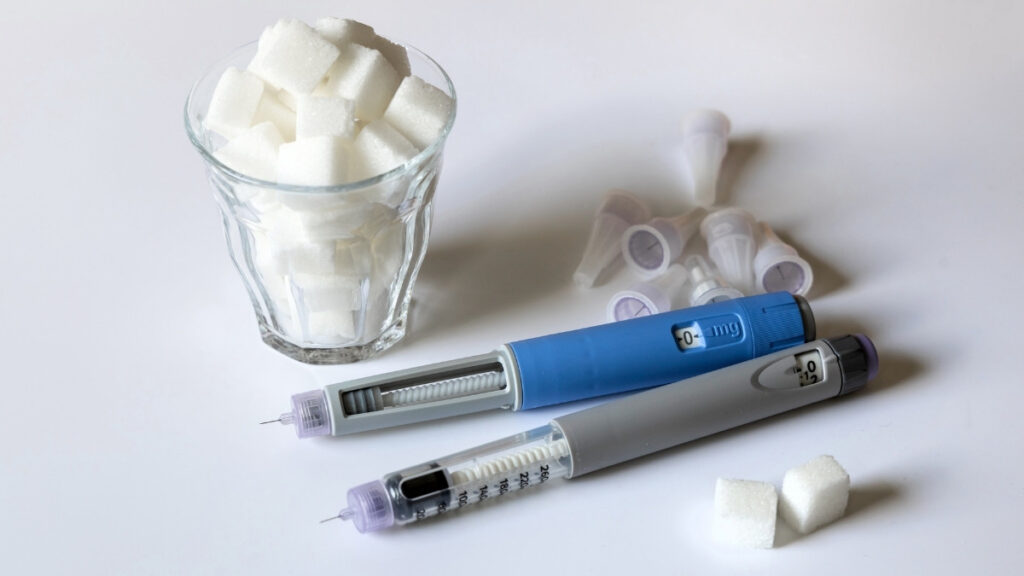
Here’s what you need to know before making any big changes.
If you take insulin or certain diabetes pills (sulfonylureas like glyburide, glipizide), your blood sugar can drop dangerously low when you change your diet. This is called hypoglycemia. It makes you shaky, sweaty, confused, and dizzy. Severe cases can make you pass out.
Never stop or change medications without talking to your doctor first.
You need extra caution if you have heart disease, kidney disease, or your BMI is already low. Dramatic diet changes can stress your body in ways you might not expect.
Seniors already get dehydrated more easily than young people. When you’re eating less or fasting, you need to drink more water. Not soda. Not juice. Plain water.
Watch for These Warning Signs
Check your blood sugar more often when you start a new eating plan. If it drops below 70, eat something with quick sugar (juice, glucose tablets, regular soda).

Signs of low blood sugar:
- Shaking or trembling
- Sweating when you shouldn’t be
- Feeling confused or irritable
- Rapid heartbeat
- Extreme hunger suddenly
On the flip side, very high blood sugar also affects your brain. Both extremes are bad for thinking clearly.
Your Doctor Is Your Partner

The new 2025 guidelines from the American Diabetes Association emphasize something important: every older adult needs an individualized approach. What works for your neighbor might not work for you.
Your doctor needs to know what you’re planning. They’ll adjust medications as your blood sugar improves. They’ll monitor for problems. They’ll celebrate your wins with you.
Don’t see this as asking permission. See it as bringing in an expert to help you succeed.
Your Step-by-Step Action Plan
Your Step-by-Step Action Plan!
Ready to start? Here’s exactly what to do.
Step 1: Talk to Your Healthcare Team This Week
Schedule an appointment. Tell them you want to work on reversing your diabetes. Ask about:
- Your current A1C, weight, and blood pressure numbers
- Which medications you take that affect blood sugar
- Whether any medications could be reduced or stopped as you improve
- What blood sugar levels are safe targets for you
Bring this article. Show them which approach interests you.
Step 2: Pick Your Starting Strategy
Don’t try to do everything at once. Pick ONE approach that fits your life:
- Can you commit to strict calorie counting? Consider the VLCD with medical supervision.
- Do you love flavorful food? Try the Mediterranean diet.
- Are you an all-or-nothing person? Intermittent fasting might click.
- Want the gentlest start? Just cut portions and add vegetables.
You can always adjust later. The best plan is the one you’ll actually follow.
Step 3: Start Small and Build Up
Don’t shock your system. Ease in over several weeks.
If you’re trying intermittent fasting, start with 12:12 for two weeks. Then move to 14:10. Then 16:8.
If you’re changing what you eat, swap one meal first. Make breakfast Mediterranean-style for a week. Then add lunch. Then dinner.
Add exercise gradually too. Even 10 minutes counts. Walk during one commercial break. Then two. Then three. Build momentum.
Step 4: Track Your Progress
Get a simple blood glucose monitor. Check your blood sugar at the same times each day. Write it down.
Weigh yourself weekly, not daily. Water weight swings will drive you crazy if you check every day.
But also notice how you feel. More energy? Thinking clearer? Sleeping better? These matter as much as the numbers.
As your blood sugar improves, tell your doctor. They’ll adjust medications. This is success, not a problem.
Step 5: Find Your Support System
The CDC’s Diabetes Prevention Program is free or low-cost and available in most communities. Real classes with real people. Structured guidance. Proven results.
Tell your family what you’re doing. Ask them to join you for walks. Make them your accountability partners.
Join a diabetes support group. Online or in-person. Hearing others’ struggles and wins keeps you motivated when things get hard.
Don’t Make These Mistakes

Starting a very restrictive diet without telling your doctor? Dangerous. Your medications need adjustment as your blood sugar changes.
Stopping your medications because you feel better? Also dangerous. Your blood sugar might feel fine because the medication is working. Stop it suddenly and you could end up in the emergency room.
Not eating enough nutrients during restricted eating? You’ll feel terrible and quit. Make sure you’re getting protein, vitamins, and minerals even if you’re eating less.
Comparing your progress to someone 30 years younger? They have different bodies, different metabolisms, different lives. Your only competition is yesterday’s version of you.
Expecting instant results? Real, lasting change takes 6-12 months. If someone promises faster, they’re selling something.
Believing products that claim to “cure” diabetes? If it sounds too good to be true, it is. No supplement, no tea, no special powder will cure diabetes. Only proven lifestyle changes work.
Sticking with an approach that clearly isn’t working? If you’ve given something an honest 3-month try and it’s making you miserable or not helping, try something else. There’s more than one path to the same destination.
Your New Reality Starts Today
Martha lost 35 pounds over 8 months. Her A1C dropped from 8.2 to 5.4. She’s off all diabetes medication. She’s 69 now and says she feels better than she did at 60.
Your story could be next.
Age isn’t holding you back. In fact, adults over 60 show better results than younger people in diabetes prevention programs. You have life experience. You know yourself. You can make decisions and stick with them.
Multiple approaches work. Pick one that fits your life. Start with the smallest change you can maintain forever, not the biggest change you can do for a week.
Medical supervision matters, but it’s not a barrier. Your doctor wants you to succeed. Work together. Track your progress. Adjust as needed.
Small changes add up. Walk 10 minutes today. Eat one more vegetable. Skip the soda. Do it again tomorrow. In three months, you’ll look back and barely recognize the person you were.
What to Do Right Now
Pick up your phone. Call your doctor’s office. Schedule an appointment for this week or next.
Choose ONE dietary change to start Monday. Just one. Make it small enough that it feels easy.
Find someone to be your walking buddy. A friend, your spouse, your neighbor. Ask them today.
Download a blood sugar tracking app or buy a simple notebook. Start writing down your numbers.
Reversing type 2 diabetes after 60 isn’t just possible. For many seniors, it’s become their new reality. The path to diabetes remission starts with a single conversation with your healthcare provider.
The question isn’t whether you can do this.
The question is: when will you start?








