7 Biggest Reasons For Poor Balance With Aging & How To Fix (According to the Expert Trainers)
If you’ve noticed yourself feeling less steady on your feet after age 50, you’re not imagining it—and you’re definitely not alone. That increased unsteadiness when walking, the fear of falling, and the hesitation you feel navigating stairs or uneven surfaces are common balance problems as you age.
But here’s the empowering truth: balance decline isn’t inevitable. In this guide, you’ll discover the seven specific reasons your stability decreases after 50, along with evidence-based exercises to address each one.
Best of all, these fall prevention solutions take less than 10 minutes daily and require no expensive equipment. By understanding what’s causing your balance issues, you can improve stability, regain confidence, and maintain your independence for years to come.
Why Balance Matters More Than You Thin
You’re standing on one foot to put on your sock. Suddenly, you wobble. You grab the wall. Your heart races a bit.
7 Reasons Your Balance Declines
Click an icon to see the problem and the 10-minute fix!
Click any icon above to see why your balance is off and how to fix it!
1. Vision Changes
Blurry vision & poor depth perception trick your brain. Dim lighting makes it worse, causing you to misjudge steps and curbs.
Schedule your annual eye exam. Walk through your home and upgrade dim bulbs to bright LEDs. Add night-lights to hallways and bathrooms.
2. Inner Ear Health
Your “balance control center” is off. Vertigo (BPPV) from stuck ear crystals, or even earwax, can cause severe dizziness.
See a doctor for any dizziness. Ask them to check for earwax. If you have BPPV, ask your doctor or a PT to teach you the Epley maneuver.
3. Poor Posture
“Tech neck” or slouching shifts your center of gravity forward, keeping you permanently off-balance and straining your back.
Wall Posture Check: Stand with your back to a wall. Gently try to touch your shoulders and the back of your head to the wall. Hold for 30 seconds. Repeat 3 times daily.
4. Wrong Shoes / Numb Feet
Thick, cushy shoes or foot numbness (neuropathy) blocks signals from your feet to your brain. You can’t “feel” the ground.
Corner Balance Practice: Stand in a room corner for safety. Practice balancing with feet together, then on one leg. Hold for 30 seconds. Repeat 3 times.
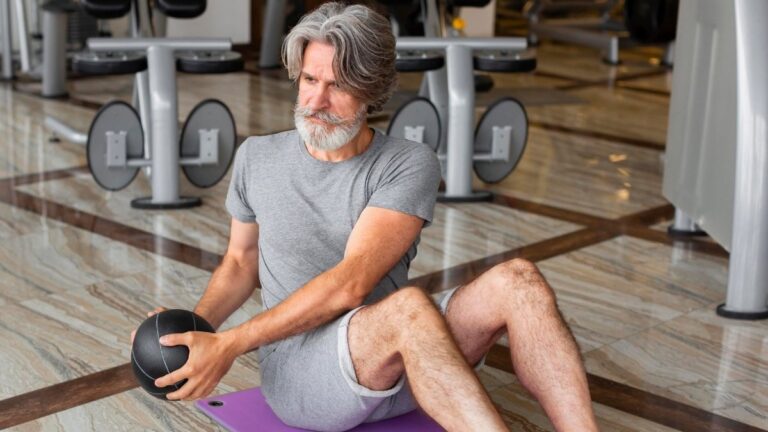
5. Neglecting Leg Strength
Natural muscle loss (sarcopenia) means your legs are too weak to “catch you” when you stumble or to get up from a chair easily.
Sit-to-Stands: Sit in a sturdy chair. Stand all the way up and sit back down slowly, 10-15 times. Try not to use your hands!
6. Staying on Flat Surfaces Only
You only walk on flat sidewalks, so your brain forgets how to handle uneven ground (like grass, gravel, or trails).
“Use it or lose it.” Spend 10 minutes walking on the grass in your yard or a local park. Notice how your ankles have to work differently.
7. Never Practicing “Awkward” Moves
Most falls happen when moving *sideways* or *backward*. We stop practicing these, so we panic and fall when caught off guard.
Sidestepping: Hold onto your kitchen counter for support. Take 10 steps to the right, then 10 steps to the left. Repeat 3 times.
That moment? It’s your body sending you a message.
Falls kill more adults over 65 than any other injury. [INSERT: Current CDC statistics on fall-related injuries in adults 65+]. The medical bills hit hard too—[INSERT: Cost of fall-related medical treatments 2024-2025].
At 55, I noticed I couldn’t stand on one foot for more than three seconds. I stopped going to crowded places because I was scared of getting bumped. I didn’t tell anyone. I just… stopped doing things.
Here’s what most people don’t know: Balance doesn’t have to decline with age. It declines when we stop challenging it.
The seven mistakes below steal your balance without you noticing. Fix them, and you can get your stability back in weeks, not months.
1. Ignoring Vision Changes
Your eyes and your balance are connected in ways you probably don’t expect.
When your vision gets blurry, your brain can’t judge distances correctly. That curb looks flat. That step looks closer than it is. Your brain guesses wrong, and down you go.

The depth perception problem: Each year after 50, your eyes process visual information a bit slower. You lose some peripheral vision. Colors don’t contrast as sharply. [INSERT: Statistics on vision-related falls in older adults]. Many adults walk around with outdated prescriptions and don’t realize how much it affects their stability.
Think about walking from your bright living room into a dark hallway at night. Your eyes need time to adjust. During those few seconds, you’re basically walking blind. That’s when accidents happen.
What makes this sneaky: Vision changes happen so slowly that your brain compensates. You lean forward more to see better. You grab railings you didn’t need before. You avoid walking at night. These become habits before you notice the real problem—your eyes.
Cataracts cloud your lens. Macular degeneration steals your central vision. Reduced contrast sensitivity makes it hard to see where the floor ends and the carpet begins. One patient told me she tripped over her black cat on her dark gray rug five times before getting new glasses.
The lighting factor: Dim lighting makes everything worse. Shadows trick your brain. Glare from windows blinds you temporarily. Studies show that improving home lighting reduces falls by up to 40%.
What You Need to Do
Schedule an eye exam every year after 50. Not every two years—every year. Vision changes fast at this age.
Update your glasses as soon as your prescription changes. Don’t wait because your current glasses “still work okay.”
Light up your home properly. Put bright LED bulbs in hallways. Get motion-sensor lights for bathrooms. Add night lights along your path from bedroom to bathroom.
Increase contrast in your home. Put bright tape on the edges of steps. Use light-colored rugs on dark floors, or dark rugs on light floors.
Mark the edges of steps with bright yellow or white tape. It sounds simple, but it works.
Bonus tip: Clean your glasses every morning. Smudged lenses reduce clarity more than you think.
2. Neglecting Your Inner Ear Health
Your inner ear does more than help you hear. It’s your balance control center.
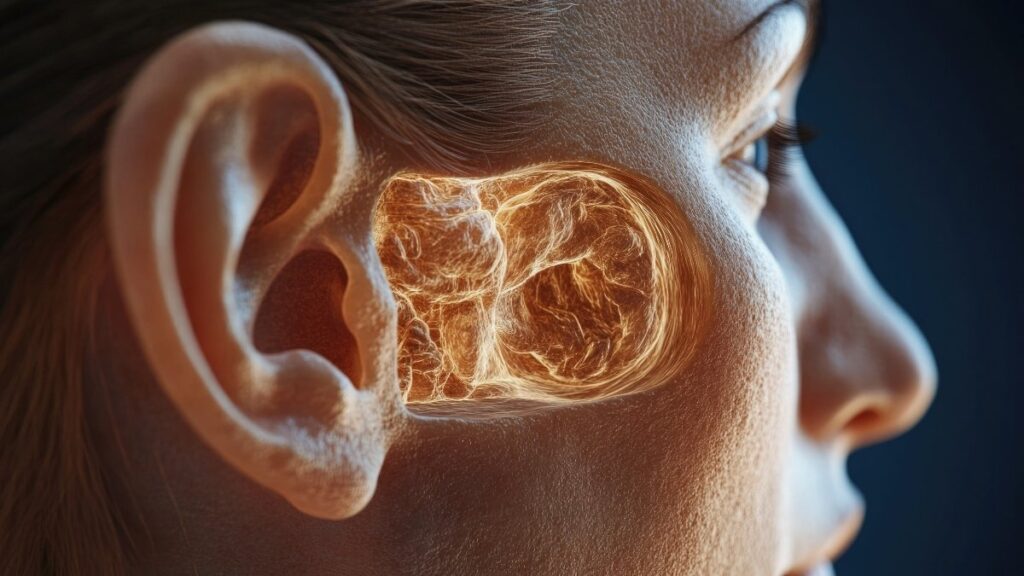
Inside your ear sits the vestibular system—three tiny loops filled with fluid and crystals. When you move your head, the fluid shifts. The crystals roll around. This tells your brain which way is up. It happens automatically, thousands of times a day.
When things go wrong: Ear infections throw this system off, even after the infection clears. The fluid gets thicker. The crystals get stuck in the wrong place. Suddenly, the room spins when you roll over in bed.
Benign Paroxysmal Positional Vertigo (BPPV) is the most common cause of vertigo in adults over 50. [INSERT: Statistics on BPPV in adults over 50]. Those tiny crystals drift into the wrong canal. Your brain gets confused signals. You feel like you’re on a boat in a storm, but you’re just lying in bed.
The earwax surprise: Impacted earwax pushes on your eardrum. This creates pressure that messes with your balance system. You feel off-balance but can’t figure out why. A simple professional ear cleaning fixes it in minutes.
Medications you take every day might be the culprit: [INSERT: Common medications that affect balance – blood pressure meds, certain antibiotics]. Some blood pressure medications cause dizziness. Certain antibiotics damage the inner ear. Even common pain relievers can affect your vestibular system when taken long-term.
Watch for these symptoms:
- The room spins when you turn your head quickly
- You feel dizzy when you lie down or sit up
- You have trouble walking in the dark
- You feel foggy or confused (inner ear problems can cause this)
- You veer to one side when walking
What You Need to Do
See your doctor if you experience any dizziness or vertigo. Don’t wait for it to get worse.
Get professional ear cleanings if you produce a lot of earwax. Don’t use cotton swabs—they push wax deeper.
Review all your medications with your doctor. Ask specifically, “Could any of these affect my balance?”
Learn the Epley maneuver for BPPV. This simple head movement repositions those crystals. Your doctor or a physical therapist can teach you. [Link to demonstration video].
Consider vestibular rehabilitation therapy if problems persist. Physical therapists who specialize in this can retrain your balance system.
Expert insight: [INSERT: Quote from ENT specialist or physical therapist specializing in vestibular disorders about connection between ear health and falls]
3. Living With Forward-Slouched Posture
Look down at your phone right now. Feel how your head tips forward? Your neck tenses up?
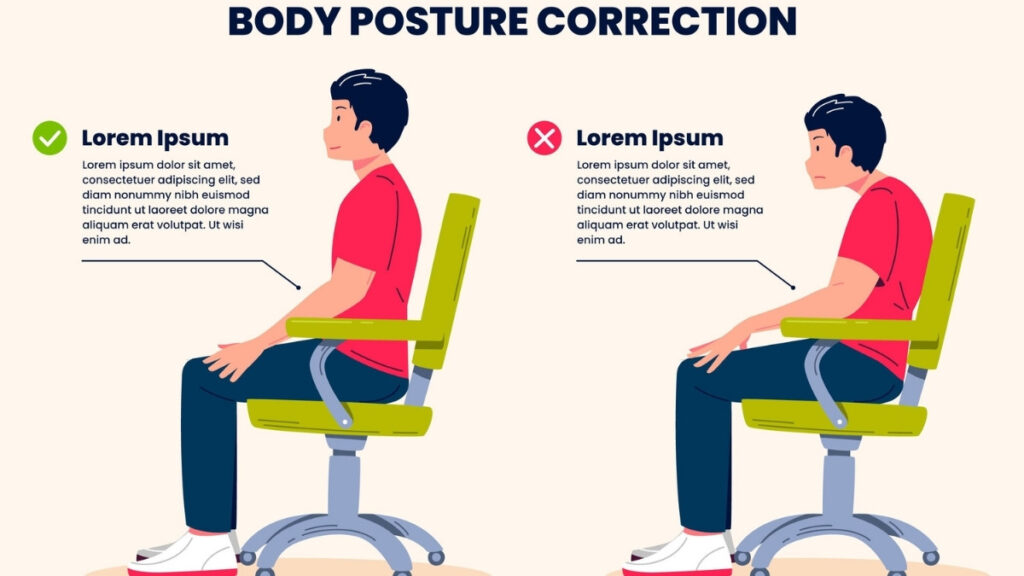
That’s killing your balance.
Here’s why: Your head weighs about 10-12 pounds. When it sits directly over your spine, your body handles the weight easily. But for every inch your head moves forward, you add 10 pounds of pressure to your spine. Tilt forward three inches, and your neck holds up 40 pounds.
This shifts your center of gravity forward. Your body compensates by leaning more. Your muscles work harder. You feel tired. Your back hurts. And you’re way more likely to fall forward.
The tech neck epidemic: We spend hours looking down at phones, tablets, and laptops. This creates a forward curve in your upper back called kyphosis. [INSERT: Statistics on kyphosis in older adults]. Over time, the curve becomes permanent. Your muscles get weak and tight in all the wrong places.
What happens to your balance: When you stand up straight, your body naturally balances. Your core engages. Your hips align. Your weight distributes evenly across both feet. But with forward head posture, everything shifts. Your feet work harder to keep you upright. Your ankles wobble more. You tire faster.
Bonus problem: Poor posture squeezes your lungs. You can’t breathe as deeply. Less oxygen means less energy. Less energy means weaker muscles. Weaker muscles mean worse balance. It’s a downward spiral.
Think about the last time you had back pain. Did you notice you walked more carefully? Took smaller steps? That’s because pain changes how you move, which further wrecks your balance.
Wall Posture Check Exercise
This simple exercise shows you how far your posture has drifted. It also helps correct it over time.
How to do it:
Stand with your buttocks touching a wall. Your feet can be a few inches out from the wall—that’s fine, especially if you have balance concerns.
Bring your shoulder blades back until they touch the wall. Don’t force it. Just gently squeeze them together.
Slowly bring your head back. Tuck your chin slightly, like you’re making a double chin. You’re trying to get the back of your head near or against the wall.
Hold this position for 30 seconds. It might feel impossible at first. That’s normal.
Repeat three times daily.
What to expect:
Week 1: You might only get your shoulders back. Your head stays way forward. Don’t worry.
Week 2-4: Your head gets closer to the wall. The position feels less weird.
Month 2-3: You can hold the full position comfortably. You naturally stand taller throughout the day.
Important: Some people need weeks to months to fix severe forward posture. This isn’t a quick fix. It’s a daily practice that creates real, lasting change.
4. Wearing the Wrong Shoes (Or Having Numb Feet)
Your feet are covered in tiny sensors. They feel every bump, every texture, every shift in the ground. These sensors—called mechanoreceptors—send instant messages to your brain: “Gravel ahead!” “Slippery tile!” “Uneven surface!”

This is proprioception. It’s your body’s GPS system.
The thick-sole problem: Modern athletic shoes have thick, cushy soles. They feel comfortable. But they block the signals from your feet to your brain. It’s like trying to feel the floor while wearing oven mitts. You lose critical information about the ground beneath you.
[INSERT: Statistics on peripheral neuropathy in adults over 60]. Many adults over 60 have reduced sensation in their feet. Add thick shoes to numb feet, and you’re basically walking blind.
Diabetic neuropathy: Diabetes damages the nerves in your feet over time. [INSERT: Percentage of diabetics with foot neuropathy]. You can’t feel the floor properly. You don’t notice when you step on something sharp. You can’t tell if you’re about to roll your ankle. This dramatically increases fall risk.
Other causes of foot numbness:
- Vitamin B12 deficiency (common in older adults)
- Peripheral neuropathy from other conditions
- Tight shoes that reduce circulation
- Sitting with crossed legs too long (crushes nerves)
The barefoot shoe debate: Some experts recommend minimalist or “zero drop” shoes that let your feet feel the ground better. Studies show improved balance and foot strength. But this isn’t right for everyone.
If you have plantar fasciitis or serious foot problems, you need support. The key is finding the right balance between protection and ground feel.
Proprioception Exercises: Corner Balance Practice
This exercise rebuilds the connection between your feet and your brain.
Why use a corner: You have walls on three sides. You feel safe. You can grab the wall anytime you wobble.
Equipment: A cane, walking stick, or sturdy chair works too. Place it in front of you for extra support.
Progression 1: Feet Together
Stand in the corner with feet together. Hold onto something if needed.
Try to let go and balance for 30 seconds. Watch your ankles wobble back and forth. That wobbling? That’s proprioception working. Your feet are sending signals. Your brain is adjusting.
Do this 3 times. Rest between sets.
Progression 2: Single Leg Stands
Stand in the corner. Hold onto support.
Lift one foot off the ground. Just an inch is fine. Try to balance for 30 seconds.
Switch legs. Do 3 repetitions on each leg.
Advanced: Add a Balance Pad
Once you can do single-leg stands easily, add a cushion or balance pad. This makes your feet work even harder to stabilize you.
Do the same progressions: feet together, then single leg.
What to notice: Your feet constantly make tiny adjustments. Your toes grip the floor. Your ankles shift. This is exactly what you want. You’re retraining your proprioception system.
Shoe Recommendations
If you have foot problems or plantar fasciitis: Prioritize support. Get proper arch support and cushioning. Your feet need help healing before you challenge them.
If you’re generally healthy: Consider thinner athletic shoes with moderate support. You don’t need to go full barefoot. Just choose shoes that let you feel the ground a bit more.
A good compromise: Look for shoes with thinner soles but still have good fit and some support. Think hiking shoes rather than running shoes.
Around the house: Walk barefoot or in socks on carpet sometimes. This gives your feet direct feedback. Just watch for trip hazards.
5. Skipping Leg Strength Training
After age 30, you lose muscle naturally. It’s called sarcopenia. By age 50, the loss speeds up. [INSERT: Statistics on muscle loss after age 50].

Why this destroys balance: Weak legs can’t catch you when you stumble. Weak hips can’t stabilize your pelvis. Weak ankles collapse inward or outward. Each weak muscle is a potential fall waiting to happen.
[INSERT: Rate of strength decline in sedentary vs. active older adults]. The difference between active and inactive older adults is dramatic. Active people maintain strength for decades longer.
The confidence connection: When your legs feel strong, you move with confidence. You take stairs without gripping the railing. You carry groceries without fear. You get in and out of cars easily. This confidence makes you more active, which makes you stronger. It’s a positive cycle.
Real-world signs you need leg strength:
- You push with your hands to stand up from a chair
- Climbing stairs makes your legs burn
- You avoid carrying heavy grocery bags
- Getting in and out of a car feels hard
- You sit down heavily instead of lowering yourself slowly
The good news? You don’t need a gym. You don’t need equipment. Your body weight is enough.
Essential Leg Exercises
Do these 3-4 times per week. They take 10-15 minutes total. Use a sturdy kitchen chair for support.
Exercise 1: Sit-to-Stand
Sit in a chair. Your feet should be flat on the floor.

Cross your arms over your chest. This prevents you from pushing with your hands.
Stand up using only your legs. No leaning forward excessively. No pushing off the chair.
Sit back down slowly. Control the descent. Don’t plop down.
Do 10-15 repetitions. If you can’t do it without hands at first, use them. Work up to no hands.
Why this matters: This mimics real life. You sit and stand dozens of times daily. Stronger legs make this effortless.
Exercise 2: Calf Raises
Stand behind a chair. Hold the back for balance.

Rise up onto your toes as high as you can. Hold for 2 seconds.
Lower back down slowly. Feel your calves working.
Do 15-20 repetitions.
Why this matters: Your calves control ankle stability. Strong calves prevent ankle rolls and twists.
Exercise 3: Standing Marches
Stand next to a chair or counter. Hold on lightly for balance.

Lift one knee up high, like you’re marching. Bring it as high as you comfortably can.
Lower it. Lift the other knee.
Do 20 marches on each leg (40 total).
Why this matters: This builds hip flexor strength. Hip flexors lift your leg with each step. Weak hip flexors cause shuffling, which causes trips.
Progression Over Time
Week 1-2: Do one set of each exercise. Use support when needed.
Week 3-4: Add a second set. Try using less support.
Week 5-8: Add a third set. Challenge yourself to go slower, which makes it harder.
Important note: Start where you are. Using hands for support is perfectly fine initially. The goal is progress, not perfection.
6. Staying on Flat, Even Surfaces Only
Your brain is like a muscle. Use it, and it gets stronger. Stop using it, and it weakens.

Balance works the same way.
Walking on smooth sidewalks every day teaches your brain one thing: how to walk on smooth sidewalks. But real life isn’t smooth. Real life has cracks, curbs, gravel, grass, and uneven pavement.
The “use it or lose it” principle: Your brain creates neural pathways for movements you practice. [INSERT: Research on varied terrain training and fall reduction]. When you only walk on flat ground, those pathways stay simple. When you walk on varied terrain, your brain builds complex pathways. More pathways equal better balance.
The mental health bonus: Outdoor walking in nature reduces stress hormones. It lowers blood pressure. It improves mood. Studies show people who walk in nature have better mental health than people who walk on treadmills. And better mental health means you stay more active, which circles back to better balance.
Why hiking poles help: They’re not just for serious hikers. Poles give you two extra points of contact with the ground. They help on uneven terrain. They reduce impact on your knees. They make you feel secure enough to try more challenging walks.
Progressive Challenge Levels
Start at your level. Progress as you feel comfortable. There’s no rush.
Level 1: Beginner
Walk on grass in your backyard. Notice how your feet sink slightly. Your ankles adjust with each step.

Walk on your gravel driveway. The uneven surface forces tiny balance corrections.
Walk on different floors in your home. Notice how carpet feels different from hardwood or tile.
Level 2: Intermediate
Find a nature trail with gentle inclines. State parks often have easy trails marked “beginner.”

Walk on a sandy beach if you live near one. Sand challenges your balance significantly.
Walk on mulch paths in parks. The soft, shifting surface builds ankle strength.
Level 3: Advanced
Try hiking trails with roots and rocks. You’ll step over obstacles, duck under branches, and navigate uneven ground.

Walk on cobblestone streets if your city has them. The constant irregularity builds balance.
Try forest paths where you can’t always see the ground clearly. Your proprioception takes over.
Safety Recommendations
Use walking sticks or trekking poles. They help tremendously on uneven ground.
Go with a friend or family member. Company is safer and more fun.
Stay on marked trails. Don’t get adventurous until you’re confident.
Check weather conditions. Wet trails are slippery. Hot days are exhausting.
Tell someone your route and when you’ll be back. Basic safety.
Start with short walks—10-15 minutes. Build up duration as you gain confidence.
7. Never Practicing “Awkward” Movements
Most falls don’t happen when you’re walking forward. They happen when you step backward, sidestep in a crowded kitchen, or turn around quickly to answer the door.

These are called perturbations—unexpected movements that catch you off guard.
Why we avoid them: These movements feel uncomfortable. They require more concentration. So we eliminate them from our lives without realizing it. We turn our whole body instead of just our head. We take extra steps forward instead of stepping backward. We create habits that make us safer in the short term but more fragile in the long term.
The panic reaction problem: When you rarely practice backward walking, your body doesn’t know how to react when it needs to. You panic. Your muscles tense up. You overcorrect. And you fall.
[INSERT: Statistics on falls during “unexpected movements”]. [INSERT: Most common locations for indoor falls – kitchen, bathroom]. Falls happen in familiar places doing ordinary things because those are the places where unexpected movements occur.
The sideways fall danger: Falls directly sideways are particularly dangerous for hip fractures. Your hip bone hits the ground with full force. Practicing sideways movements teaches your body how to catch itself.
Daily Practice Routines (5-10 Minutes)
Do these along your kitchen counter, bathroom railing, or anywhere with solid support. Never practice without something to grab.
Exercise 1: Sidestepping
Hold onto your countertop or railing with both hands if needed.

Step sideways with your right foot. Bring your left foot to meet it.
Continue sidestepping until you reach the end of your counter.
Look straight ahead, not at your feet. This is important. In real life, you don’t look down.
Turn around and sidestep back the other direction.
Do 2-3 passes in each direction.
Why this matters: You sidestep in kitchens, crowded hallways, when someone walks past you. This makes it automatic instead of scary.
Exercise 2: Forward March + Backward Walk
March forward along your counter with high knees. Take 10-15 steps.
At the end, turn around and walk backward slowly. Keep one hand on the counter.
This simulates going up stairs (forward march) and backing into a chair (backward walk).
Do 2-3 passes.
Why this matters: Backing into chairs causes many falls. Walking backward with control makes it safer.
Exercise 3: Grapevine/Karaoke (Advanced)
This one is tricky. Skip it if it feels too confusing or unstable.
Stand next to support. Cross your right foot in front of your left. Step.
Cross your right foot behind your left. Step.
Continue this pattern: front, behind, front, behind.
Go one direction, then reverse.
Why this matters: This trains your brain to handle complex foot patterns. It’s like insurance for when you need to make a weird movement quickly.
Exercise 4: Heel-Toe Walk
Walk in a straight line along your counter. Place your heel directly in front of your other foot’s toes. Heel touches toe each step.
It’s like walking a tightrope.
Try it backward for an extra challenge. This is hard. That’s good.
Focus on the feeling of your heel making contact with your toe. Concentrate on the physical sensation.
Frequency: Daily if possible. This routine takes 5-10 minutes.
Location: Anywhere with support. Kitchen counter works great. Bathroom railing. Hallway with wall support.
Safety: Never do these exercises without support nearby. The point is to challenge yourself safely, not risk a real fall.
Creating Your Personal Balance Improvement Plan
You don’t need to fix everything at once. That’s overwhelming and doesn’t work anyway.
Instead, figure out which issues apply to you. Then tackle them one or two at a time.
Assessment Checklist
Go through this honestly:
☐ When did I last have an eye exam? Has it been more than 2 years?
☐ Do I experience any dizziness, vertigo, or room-spinning sensations?
☐ Do I slouch forward when standing or sitting? (Check with the wall test)
☐ Do I have numbness, tingling, or reduced sensation in my feet?
☐ Do I struggle to rise from a chair without using my hands?
☐ Do I only walk on flat, even surfaces like sidewalks and indoor floors?
☐ Do I avoid moving sideways or backward? Does it feel scary or awkward?
Your priorities: Check marks mean focus here first. Start with the issues that apply most directly to you.
Timeline Expectations
Be realistic. Balance doesn’t improve overnight. But it improves faster than most people think.
Week 1-2: Try the exercises. See which ones feel right for your body. Some will feel easy. Some will feel hard. Both are useful information.
Week 3-4: You’ll notice improved confidence. You might stand on one foot while brushing your teeth without thinking about it. You might walk through a crowded room without anxiety.
Month 2-3: Measurable strength and balance gains appear. You can hold single-leg stands longer. You can do sit-to-stands without hands. Friends might comment that you’re standing taller.
Month 3-6: Significant fall risk reduction. Your body automatically catches itself when you stumble. You move with confidence. You try activities you’ve been avoiding.
When to See a Professional
Some situations require expert help. Don’t try to handle these on your own:
See a doctor or physical therapist if:
- You’ve had a fall in the last 6 months
- You experience sudden balance changes that weren’t there before
- You have persistent dizziness that doesn’t improve
- You can’t safely do these basic exercises even with support
- You have a medical condition that affects balance (stroke, Parkinson’s, MS)
Physical therapists who specialize in balance and fall prevention can assess your specific situation. They can create a personalized plan. Insurance often covers this.
Start Small, Start Now
Balance decline isn’t inevitable. It’s not “just part of aging.” It’s a result of specific, fixable problems.
You’ve just learned seven causes and seven solutions:
- Get your vision checked and improve lighting
- Address inner ear issues and review medications
- Improve your posture with daily wall checks
- Rebuild foot sensation and wear appropriate shoes
- Strengthen your legs with simple exercises
- Walk on varied terrain regularly
- Practice awkward movements daily
You don’t need hours. You need 15 minutes a day and consistency.
The benefits go beyond fall prevention. You’ll stand taller. Move with confidence. Feel less pain. Maintain independence longer. Keep doing the activities you love.
Your action step for today: Choose just ONE area from the list above. Not three. Not all seven. One.
Schedule that eye exam. Stand against the wall and check your posture. Spend 5 minutes sidestepping along your kitchen counter. Walk across your grass instead of staying on the sidewalk.
Small, consistent actions create significant results. Your future self—the one who stays active, independent, and confident—will thank you for starting now.